Mis à jour le Jeudi, 13 Février 2020
Part 1 of 5 | Children and Adolescents’ Mental Health Services (CAMHS) & Learning and Intellectual Disabilities

CAMHS deal with the psychological issues of people under the age of 18. They are a non-specialist service and often refer to other more specialised departments following the initial assessment of patients. The most common cases tend to be adolescents with depression and anxiety whose manifestations are not different to those of adults and so are treated fairly similarly.
Inclusivism in Learning Disabilities
In 1969, Bengt Nirje adopted and developed the concept of normalisation in Sweden and beautifully described it as…
“making available to all mentally retarded people patterns of life and conditions of everyday living which are as close as possible to the regular circumstances and ways of life of society.”
– Nirje, 1980
Learning Disability is not just an impairment in Cognition
The social impairment of Learning Disabilities – US Statute 111 – 256: Rosa’s Law defines the factual impairment, the imposed or acquired disability and the awareness of being different.
The Normalisation Theory
This theory focuses on the mainstream trends of social devaluation or deviancy making. Some categories of people tend to be valued negatively due to their behaviours, appearances and characteristics, and this places them at the risk of being devalued [according to the Normalisation Theory of Nirje on the societal processes he assumed] – people fulfil various social roles and stereotypes.

As part of the deviancy making or social devaluation, the unsophisticated minds of the masses generally do not mean to stereotype, however they seem to do it unconsciously [the unconscious is a concept Sigmund Freud and Jacques Lacan acknowledged in their psychoanalytic theories of mental/psychological activity and mental health problems linked to psychopathic tendencies in people towards others], i.e. deviant groups with social symbols or images that are at a higher risk of being devalued are the focus of the normalisation theory, which is believed to be done with the aim of providing them with the skills they need and eventually change the status of these deviant groups to functional members of society.
Lutte contre l’illettrisme En 6ème, je ne savais pas écrire mon nom ! (2016)
Society tends to distance itself from deviant groups without any purpose or belonging, however psychologists provide support for the social integration and valued social participation of people with learning disabilities through exercises that involve learning through imitation. This challenges stereotypes within wider society through direct experiences of spending time with people who are affected by learning disabilities.
While psychology evolves and sophisticated and modern theories about intelligence and communication such as our “Organic Theory” take shape, we hope that observations such as this one may be digested and understood by the masses, that is:
“While the communicative patterns [language] in human primates vary with socio-behavioural and geographical patterns; creativity and IQ remain constant and do not change. Intelligence and creativity cannot be stopped because of linguistic differences, since talented and gifted humans do not choose the location of their birth nor their linguistic heritage but still contribute to the enhancement of our civilisation.”
Which concludes that that the intelligence of an invidual when assessed on a range of variables [e.g. perception, fluid intelligence, artistic creativity, reasoning, emotional intelligence, courage, values, etc] cannot be deduced by simply assessing their academic abilities, since human life has various sides to itself. Hence, the true worth and value of an individual may always remain a problem and a mystery to fully assess [since most only assess people on the variables they are interested in, for e.g. a company looking for a secretary will assess the applicant on her ability to handle office politics, and not other abilities essential to exist as a human within civilisation], and this seems to go in line with Jean Piaget’s deduction about the uniqueness of the human organism and mind.

“I am still learning” – Michael-Angelo at the age of 87 / Image: La Création d’Adam (1508 – 1512)
Neurodevelopmental Disorders & Intellectual Disabilities
Neurodevelopmental disorders are disorders occurring due to the biological dysfunction of the brain that in turn lead to developmental deficits that come in a range that can be very specific to global impairment. These groups however often co-occur together, i.e. one could be affected with Intellectual Disability (ID) and also Autistic Spectrum Disorders. Psychologists are expected to show great care when assessing this group of disorder as they vary in severity. Severity has 4 Specifiers and 3 Domains [Intellectual].
Specifiers: [1] Mild – [2] Moderate – [3] Severe – [4] Profound
Domains [Intellectual]: [1] Conceptual – [2] Social – [3] Practical
Intellectual Domains
The first domain, which is the Conceptual Domain refers to all things learnt at school and required for employment and adequate independent functioning within the community. Secondly, the Social Domain refers to social, developmental and emotional factors associated to age. This manifests in them as being victims of manipulation and abuse by others. Finally, the Practical Domain refers to all skills required to live healthily [also this is subject to interpretation depending on contexts, socio-linguistic and cultural settings].
Intellectual Disability
For one to be qualified as intellectually disabled, we would have to meet all the 3 criteria below:
- Deficits in intellectual functions, such as reasoning, problem-solving, planning, abstract thinking, judgement, learning [also from experience].
- Deficits in adaptive functioning that means failure to meet developmental milestones within the socio-cultural standards. Limited function in daily life, participation, communication, independence in multiple environments (i.e. Global).
- Onset is during developmental period [childhood – another link to the Psychoanalytic theory of Sigmund Freud & Jacques Lacan]
Assessment and Judgement
Careful distinction must be made when assessing patients suspected of suffering from Intellectual Disabilities (ID) between the low end of normal function and ID itself. The most widely used method clinically are IQ assessments and typically suggest any score that is 2 Standard Deviations below the mean [IQ scores of 75 +/-5] and whether the patient has had any clinical experience. Assessment based on the patient’s reasoning in real-life situations are also made. Global Developmental Delay is a term reserved for children under 5 who cannot adequately be assessed, but have missed all their developmental milestones.
Associated Features with Intellectual Disabilities (ID) to look for when diagnosing patients are:
- Social judgment
- Assessment of risk
- Self-management of behaviour – interpersonal relationships and emotions
- Motivation in school, university or work
- Lack of communication skills and functional problem behaviours
- Gullibility [Diagnosis is based on how people and society mistreat them – quite shocking or controversial?]
- People with Intellectual Disabilities (ID) are also at high risk of suicide
Prevalence of Intellectual Disabilities
In the UK, 1% of people suffer from intellectual disabilities and 0.006% of the population have severe disabilities requiring supported living [that is about 360, 000 people in the UK] – a slight bias with a ratio of 1.6:1 towards males; this is due to the vulnerability of the male brain.
Autism Spectrum Disorders
As psychology evolves more consideration are being given to a dimensional aspect of abnormal behaviour rather than the usual dimensional [i.e. inflexible and sometimes exaggerated in terms of descriptive precisions disregarding individual fluctuations in symptomatic manifestations] constructs of mental disorders. Autistic Spectrum Disorders (ASD) was the first mental disorder to initiate such a shift from categories to dimensions.
- Autistic Spectrum Disorders (ASD) with Intellectual Disability (ID) = Autism
- Autistic Spectrum Disorders (ASD) without Intellectual Disability (ID) = Asperger’s Syndrome
Characteristics of Autism Spectrum Disorders
ASD is characterised mainly by deficits in social communication and restricted patterns of behaviour. For a diagnosis of ASD the deficits must appear early in the developmental period [however they cannot be diagnosed until the demands of a particular task exceeds the child’s capabilities] – so more severe it is the earlier it is diagnosed [e.g. Rett syndrome].
[A] Communication in ASD
In ASD, it is common to find persistent deficits in social communication and social interaction across multiple contexts illustrated by:
- Deficits in social-emotional reciprocity, ranging from abnormal social approach. Failure to initiate or respond to social communications. Reduction in sharing interests, affect and emotions.
- Deficits in non-verbal communicative behaviours used in normal social interactions. Abnormal or no eye contact, body language or deficits in reading [understanding] gestures. A total lack of facial expression and non-verbal communication.
- Deficits in developing, maintaining and understanding relationships [e.g. from difficulties in adjusting behaviour to suit context]. Difficulties in sharing imaginative play or in making positive social acquaintances or friends. Hardly any interest in any form or peers.
[B] Behaviour in ASD
It is also fairly normal to notice restricted, repetitive patterns of behaviour, interests, or activities manifested by at least two of the following:
- Stereotyped or repetitive motor movements, use of objects, or speech
- Insistence on sameness, inflexible adherence to routines, or ritualised patterns of behaviour. Shows extreme distress at small changes, difficulty in transition, rigidity, insistence on same route taken or foods
- Hyper or hypo-reactive to sensory inputs or unusual interest in sensory aspects of the environment (indifference or hyper-responsive to pain, temperature, sound, textures, excessive smelling to touching of objects, visual fascination with movements or lights.
ASD may also manifest itself with or without intellectual disability, with a similar scenario for language impairment, and can be associated with medical or genetic conditions or environmental factors [exposure]. ASD can also be associated with another neurodevelopmental, mental or behavioural disorder and can also comprise catatonia.
Features to look out for
- People with ASD often have uneven profiles or abilities – even the high functioning variants, and this can lead to substantive stress for them
- They also often have odd motor idiosyncrasies – such as an odd gait, clumsiness and abnormal ambulatory movements.
- Disruptive, challenging behaviour and injuries are also very common
- As sufferers of ASD age, they are also more prone to developing anxiety and depression and are likely to end up in a catatonic state
Prevalence
Autistic Spectrum Disorders (ASD) seem to be a genetic disorder, however it involves a variety of genes. 15% of ASD is due to a known mutation in over 90% of concordance studies with twins. Most researchers nowadays suggest that it is inherited and polygenic [lots of genes from genetic ancestry with each adding their weight to the likelihood of the disorder manifesting]. Males are 4 times more likely to suffer from ASD than females, and even high functioning adults with ASD have poor functioning, such as low rates of independent living and employment – older adults tend to become isolated and do not engage in help-seeking behaviours [note that this is different to individuals who may have a solitary personality by conscious choice or a highly selective social circle in personal relationships based on values, in ASD the patients are generally not conscious of the causes of their debilitating condition]
Specific Learning Disorders
Specific Learning Disorders are characterised by the following:
[A] Difficulties learning and using academic skills, as indicated by the presence of at least one of the following symptoms that has persisted for longer than 6 months:
(1) Inaccurate or slow reading
(2) Difficulty understanding meaning in what was read
(3) Difficulties with spelling
(4) Difficulties with written expression
(5) Difficulties mastering number sense, number facts and calculation
(6) Difficulties in mathematical reasoning
[B] The affected academic skills are substantially and quantifiably below the expected level for the chronological age causing interference with academic, occupational or daily living
[C] Learning difficulties begin during school-age years, but will only manifest itself and be diagnosed when the affected person’s capabilities are stretched by demands
[D] It is also independent and not caused by another health or psychological disorder
Specifications of Specific Learning Disorder
SLD generally involves impairment in reading, writing and mathematics. If it is mild in intensity, the person can generally compensate. Moderately affected people however cannot compensate, but will respond to specialist teaching. Finally, severe conditions require specialist teaching in a specialist school as learning will not occur without such arrangements.
Features to look out for in confirming SLD
- SLD can occur in any individual, even those classed as gifted (IQ 130+)
- It is usually diagnosed in the early years, but in higher ability individuals it may manifest in odd ways especially when their compensatory methods are undermined
- Patient generally have difficulties with motor co-ordination
- It is a life-long condition and does not improve with therapy, but has to be compensated for
- Patients also tend to have working memory deficits and keep messy environments
- Early signs include mispronouncing words, struggling to break down words into syllables
Prevalence of Specific Learning Disorders (SLD)
SLD tend to occur in premature children or among societies with a very low birth rate. It is also more common in children with parents that smoke cigarettes [nicotine?] and is 8 to 10 times higher in families with a heritability index of 0.6 and 3 times higher in males [the vulnerability of the male brain once again]. The problems it causes with attention are likely to predict problems with the mathematical and reading components of the brain. SLD usually ends with unemployment, under-employment depression, poorer mental health and suicidal behaviour – support of any kind alters all of these outcomes.
_____________________________________
Part 2 of 5 | Anxiety Disorders


Source: World Health Organisation
Anxiety disorders are linked to the development of irrational fears of situations that are not life-threatening (Antony & Stein, 2009a). The avoidance of feared situations or experiences also lead to non-adaptive behavioural patterns. People suffering from anxiety disorders generally have fears accompanied by intense physiological arousal displayed by some or all of the following features: accelerated heartbeat, sweating, trembling, sensations of shortness of breath or smothering feelings of choking, chest pain, nausea, numbness or tingling, and chills or hot flushes. Other experiences of dizziness, derealisation (feelings of unreality) or depersonalization (feelings of being detached from the self) are also present in some cases.
In contemporary psychology there are a number of distinctions made between a variety of anxiety disorders based on the developmental timing of their emergence, the classes of stimuli that elicit the anxiety, the pervasiveness and topography of the anxiety response, and the role of clearly identifiable factors in the aetiology [the cause, set of causes, or manner of causation] of the anxiety.
The six main anxiety disorders are described below.
[1] Separation Anxiety
This condition most occurs in children and is generally manifested by a recurrent and persistent fear that is aroused when separation from the parents or caregivers is anticipated or imminent (American Psychiatric Association, 2000; Furr et al., 2009; Pine & Klein, 2008; World Health Organization, 1992). The persistent, excessive worry about losing, or about possible harm befalling a parent is the main characteristic of Separation Anxiety Disorder with nightmares on the similar themes also present in some cases along with recurrent head-aches, stomach-aches, nausea and vomiting. Separation anxiety is also one of the most common causes of school refusal, and sufferers may also display a refusal to sleep without being in close proximity with the parents.
[2] Phobias
Phobic anxiety is the irrational and intense fear aroused when one is faced with an object, event or situation from a clearly defined class of stimuli which is exaggerated in terms of danger posed (American Psychiatric Association, 2000; Blackmore et al., 2009; Hofmann et al., 2009; World Health Organization, 1992). When the person affected is exposed to the phobic stimulus, or anticipates its exposure, panic attacks may arise in adults whereas is children this may lead to excessive crying, tantrums, freezing or clinging. The persistent avoidance of phobic stimuli in phobias is endured with intense distress and this affects an individual’s personal functioning.
In the DSM, specific phobias are subdivided into those associated with animals, injury (including injections), features of the natural environment (such as heights or thunder), in particular situations (such as elevators or flying). These specific phobias are different from social phobias and agoraphobia.
In those affected with social phobias, anxiety is generally mainly aroused by social situations [e.g. public speaking, eating in public where there is the possibility of scrutiny by others and humiliation or embarrassment as a result of acting inappropriately]. In those with agoraphobia, the condition is known to manifest itself with panic attacks in public places, such as being in a queue, or on public transport – hence, these situations tend to be compulsively avoided to prevent the reoccurrence of the panic attacks.
[3] Generalized Anxiety Disorder
One of the main characteristics in general anxiety disorder is the constant feeling that misfortunes of various sorts will occur (American Psychiatric Association, 2000; Bitran et al., 2009; Hazlett-Stevens et al., 2009; World Health Organization, 1992) and the anxiety is not focused on one particular object or situation along with difficulties controlling the worrying process and a belief that worrying is uncontrollable.
General anxiety disorder is mainly composed of nervousness, restlessness, difficulty relaxing, feeling on edge, being easily fatigued, difficulties in concentration, irritability, tearfulness, sleep disturbance and signs of autonomic over-reactivity such as trembling, sweating, dehydrated mouth, light-headedness, palpitations, dizziness and stomach discomfort. [DSM requires some or more of those symptoms to be present]
Case Example of Generalised Anxiety Disorder
Margie, a 10 year old girl was referred to the psychologist after displaying excessive tearfulness in school, the condition which had been gradually amplifying over a number of months and the bouts were unpredictable. Margie would often end up in tears while playing with her friends during break time or when spoken to by the teacher. In the family doctor’s referral letter she was described as a worrier like her mother.
Presentation
in the assessment interview Margie explained that her worries were mainly about a routine daily activities and responsibilities, she would also worry about doing poorly at school and that she had made mistakes which would later be discovered, that her school friend would not like her, that she would disappoint her parents with the way she did her household chores, that she would either be too late or too early for the school bus, that there would not be any space for on the bus and that she would forget her school books. Her worries also extended to health with frequent stomach aches.
The safety of a family also troubled her, she would worry that her house would be struck by lightning, that the river would break its banks and flood the low-lying fens where she lived, washing away her whole house. The future was also a major concern of hers as she worried about failing her exams and being unable to find a satisfactory job, and being unable to find a marital partner or marrying an inadequate person. A continuous feeling of restlessness with the inability to relax was also reported by her.
Family History
The family was very close and Margie was the eldest of four children and the only girl. It was observed during the intake interview that the mother and the father displayed symptoms of anxiety, while the former had been treated with benzodiazepines for anxiety over a number of years. The family also admitted to regularly discuss their problems about their own health and safety and their own worries about the uncertainty of the future.
The father, Oliver was employed by the insurance company and regularly have conversations at the dinner table about the accidents and the burglaries that had befallen his client, and Margie regularly participated in these conversation, being the eldest among her siblings. However the main concern of the parents was about Margie’s tearfulness which they believed was unusual along with her worries and fears which they thought as legitimate. Margie spent a lot of time with her parents’ company but also had a couple of close friends with whom she played at the weekends.
Formulation
Margie was diagnosed with generalised anxiety disorder. The precipitating factor for the condition was not apparent as it had gradually evolved over the course of Margie’s development. The referral however, was precipitated by episodes of tearfulness at school. The predisposing factors in her case comprised of a highly likely possibility of genetic vulnerability to anxiety and exposure to family culture characterised by an excessive concern with safety and oversensitivity to dangerous situations. The ongoing parental conversations about potential threats to the family’s well-being likely maintained the condition along with inadvertent reinforcement of Margie’s tearfulness at school, where her tears were responded to with considerable concern.
The protective factors in the case included good premorbid adjustment, the parents’ and the school’s commitment to solving the problem and the availability of peer group support. [This formulation is diagrammed below]

Treatment
In this particular case, treatment involved family work focused on helping Margie parents reduce the amount of time they spent discussing themes related to danger and threats to their health and safety, and increase the amount engaged in activities and discussions focused on Margie’s strengths and capabilities. The parents were also assisted in coaching Margie into learning relaxation skills and mastery oriented coping self- statements. Eventually Margie showed improvement in her adjustment in school with some reduction in anxiety and tearfulness.
[4] Panic Disorder
In panic disorders, there are recurrent unexpected panic attacks; an ongoing primary fear of further attacks; secondary fear of losing control, going insane, having a heart attack or dying (American Psychiatric Association, 2000; Ballenger, 2009; Hofmann et al., 2009; World Health Organization, 1992). Acute episodes of intense anxiety our experienced in panic attacks, and these reach a peak within 10 minutes. They are characterised by autonomy hyper arousal shown by some of the following symptoms:
– Palpitations
– Sweating
– Trembling or shaking
– Shortness of breath
– Feelings of choking or smothering
– Chest pain or discomfort
– Nausea or abdominal distress
– Dizziness
– Chills or hot flushes
– Parasthesias (Numbness or tingling sensations)
– Derealisation (Feelings of unreality)
– Depersonalisation (Feelings of being detached from oneself)
In panic disorder, patients tend perceive normal fluctuations in autonomic arousal as a stimulus that provokes anxiety, with the belief that these may signal the onset of a panic attack. During a panic attack, patients typically tend to report an irresistible urge to escape the location where the attack occurred and to avoid such situations in the future. Public settings are usually the most common location where panic attacks take place [e.g. queues, public transport, shopping mall, etc] and acute autonomic arousal is only alleviated upon escape from these places or situations – hence secondary agoraphobia often develops when the patient fears leaving the safety of their homes in case of panic attacks occurring in public settings.
[5] Posttraumatic Stress Disorder (PTSD)
Post-traumatic stress disorder (PTSD) tends to occur after a catastrophic trauma such as a terrorist attack, an armed combat/robbery, a natural or man-made disaster, a serious accident that was perceived to be potentially life-threatening for oneself or others, torture, child abuse or rape.
PTSD is mainly composed of:
– Recurrent intrusive traumatic memories
– Intense anxiety in response to these memories and ongoing hyper arousal in anticipation of their recurrence
– attempts to regulate anxiety and hyper arousal by avoiding cues that trigger traumatic memories and attempts to suppress these memories when they intrude into consciousness (American Psychiatric Association, 2000; Ehlers, 2009; Friedman, 2009; World Health Organization, 1992).
Recurrent, traumatic memories include flashbacks, nightmares, or repetitive trauma themed play in the case of children, and these occur in response to internal (psychological) or external (environmental) cues that symbolise the traumatic event or aspects of it. Since patients with PTSD tend to anticipate the recurrence of traumatic memories, they experience chronic hyper-arousal which may in turn lead to difficulties in concentration, sleep difficulties, hyper-vigilance and irritability. In PTSD, the attempts to suppress traumatic memories and the avoidance of trauma-related situations may turn out to be unsuccessful, when such a scenario occurs, the PTSD person generally experiences an increase in the frequency and intensity of past traumatic memories. Emotional numbing is also quite common in chronic cases due to the frequent attempts to keep the trauma-related memory out of consciousness – this eventually leads to the inability to recall the traumatic memories. To some this may seem like a solution but the cost is excessive since emotional numbing does not only result in the exclusion of trauma-related emotions such as anxiety and anger out of consciousness, but also tender feelings such as love and joy – which cease to be experienced by the patient.
PTSD may also lead to a subjective sense of foreshortened future to the patient and this may also be accompanied by limited involvement in his/her usual activities.
[6] Obsessive Compulsive Disorder
Obsessive Compulsive Disorder (OCD) is generally characterised by distressing obsessions and compulsive rituals that reduce the anxiety associated with those obsessions [like 2 opposing forces] (American Psychiatric Association, 2000; Matthews, 2009; World Health Organization, 1992; Zohar et al., 2009). Obsessions are stereotyped thoughts, impulses or images that are recurrent and persistent. These cause serious anxiety to the patient since they are experience as senseless, uncontrollable and involuntary, and are linked to issues such as obscenity [this does not mean that healthy people with normal sexual feelings in healthy relationships have OCD], violence and danger [for e.g. some people suffer from irrational fears of the possibility of a catastrophe occurring unless symmetry or order is maintained, or there may be fears of losing control and violently raping or assaulting others, or fears of contamination [hygienic].
These compulsions are ritualistic and repetitive accompanied by stereotyped behaviours such as hand washing, ordering and checking or mental acts such as repeating words silently [which some patients feel compelled to do to regulate the anxiety caused by the obsessions], counting or praying [this should not lead to the belief that all people with faith in God suffer from OCD]. Compulsions are generally excessive attempts or unrealistic ways to avert imagined dangers entailed by these recurrent obsessions that are debilitating and are usually recognized as pointless while repeated attempts are made to resist them [once again this seems to be linked to the unconscious yet active component of mental activity and yet again leads us to Sigmund Freud and Jacques Lacan].
Clinical Features of Anxiety Disorders
The 6 anxiety disorders listed above are classified into the domains of Perception, Cognition, Affect, Arousal, Behaviour and Interpersonal Adjustment. In regards to perception, the disorders vary in the classes of stimuli that elicit the anxiety in the patient.
i)Perception
In cases of Separation Anxiety, the separation itself is the stimulus. Where phobias are the condition present, it is specific creatures [e.g. animals], events [e.g. injury], or situations [e.g. meeting new people] that trigger the anxiety. With Generalized Anxiety Disorder [GAD], the interpretation of multiple aspects of the environment end up being interpreted as potentially threatening. Panic disorder is characterised by somatic sensations of arousal such as tachycardia being perceived as threatening since they are treated as the signals that lead to full-blown panic attacks. In people with PTSD external and internal cues that bring back memories of the trauma that led to the condition elicit anxiety. In Obsessive Compulsive Disorders (OCD) stimuli that evoke obsessional thoughts elicit anxiety [e.g. potentially dirty environments or situations may give rise to obsessional ideas about hygiene and cleanliness, and anxiety about contamination.
ii)Cognition
It is important to note that in all 6 of those listed anxiety disorders, that the central organizing theme around cognition is “detection and/or avoidance of danger”. In children with Separation Anxiety there is the irrational belief that the caregivers or parents will be harmed if the separation occurs. In people affected by Phobias there is a constant fear of being harmed by either the feared object or creature, or being in the feared situation [e.g. being bitten by a god – in the case of Dog Phobia OR being negatively judged by meaningless strangers that have no connection or impact on the life of the patient in the case of Social Phobia]. As for Generalized Anxiety Disorder (GAD), patients tend to catastrophize about any features of their environment [e.g. fears of their house being burnt down, or that they will be the victim of a car crash, or punishment for some wrongdoing, they will be forsaken by those they consider as friends, and so forth – they also believe that their worries are uncontrollable. In Panic Disorder, there is the belief that more panic attacks are imminent and that they might be fatal to the patient. In many cases secondary agoraphobia also develops as they individual develops the belief that remaining in the safety of their homes might lower the probabilities of suffering from a panic attack. As for PTSD, there is the belief that as long as the intrusive memories of the trauma are forced out of consciousness, the danger of re-experiencing the intense fear, distress and horror associated with the traumatic event that led to the condition of PTSD can be avoided. Obsessive Compulsive Disorder (OCD) generally leads to obsessions mainly concerned with dirt and contamination; catastrophes such as fires, illness or death; symmetry, exactness and order; religious scrupulosity; disgust with secretions and bodily wastes [e.g. urine, saliva or stools]; lucky or unlucky numbers and extreme, wild, violent and even dangerous sexual thoughts [risk-taking] – the neutralisation of the threat posed by specific obsession-related stimuli is believed to be achieved through being engaged in specific rituals.
iii)Affect
In all 6 of the mentioned anxiety disorders affective states generally follow the beliefs about threat and danger, and these are characterized by feelings of uneasiness, restlessness and tension. In the case of OCD, outbursts of anger may occur if the patient is restricted from executing his/her compulsive rituals or if compelled to approach the feared stimuli; and in children with Separation Anxiety Disorder (SAD) may display aggressive tantrums if compelled to stay in school without their caregivers or parents. In Post-Traumatic Stress Disorder (PTSD), on top of the affective experiences of tension and uneasiness, emotional numbing arises from repeated attempts to exclude all affective material from consciousness.
iv)Arousal
The pattern of physiological arousal varies depending on the frequency of contact with the feared stimuli. In Separation Anxiety Disorders (SAD), hyper-arousal only occurs when separation is anticipated or imminent. In the case of Specific Phobias hyper-arousal only manifests in the present of the feared object or animal. In General Anxiety Disorder (GAD), a pattern of ongoing hyper-arousal can be observed, while in Panic Disorder and PTSD it is moderate followed by brief episodes of extreme hyper-arousal – these occur during attacks in Panic Disorder and when memories of the traumatic event intrude into consciousness in PTSD. In the case of OCD, specific cues related to the obsessions evoke acute and intense episodes of arousal.
In somatic symptoms the extent to which physiological arousal finds expression varies, for e.g. recurrent abdominal pain and headaches are quite common in Separation Anxiety. Sleep problems also occur in most Anxiety Disorders. In Panic Attacks it is also common to notice full blown attacks with sweating, feelings of choking or smothering, shortness of breath, trembling, nausea, dizziness, chest pains, hot flushes or chills, parasthesias, depersonalization or derealisation.
v)Behaviour
All Anxiety Disorders are characterized by avoidance behaviours, and in Specific Phobia, avoidance may even lead to a constriction in lifestyle [using an Injury Phobia as example, the patient may refuse to take part in any form of physical activity [e.g. sports] or ride a bicycle]. In other cases, the patient sometimes become house bound due to his compulsive avoidance, and this generally occurs in Separation Anxiety Disorder, Generalized Anxiety Disorder, Panic Disorder and PTSD. In those with PTSD, the use of alcohol or drugs to alleviate negative affect and suppress traumatic memories is quite common; and in OCD the patients generally engage in compulsive rituals in a desperate effort to regulate their anxiety associated with obsessional thoughts [it may be fair to note the relation between the Anxiety [as the Signifier] and the Obsessional Thoughts [as the Signified] in a Lacanian perspective here to point out the logic behind the flamboyant Frenchman’s model of Mental Activity based on Freud’s initial Topological Model – the Unconscious, the Preconscious and the Conscious]. These compulsions in OCD genereally include washing, repeating a particular action, checking, removing contaminants, touching, ordering and collecting.
vi)Interpersonal Adjustment
All 6 Anxiety Disorders affect interpersonal adjustment in a precise manner. In cases of Simple Phobia, interpersonal difficulties arise only in those situations where the individual does not conform or co-operate with normal activities [deemed social] so as to avoid the feared stimuli [e.g. a brief episode of marital conflict may occur if a husband refuses to enter an elevator at a shopping mall because of his claustrophobia]. Separation Anxiety Disorder (SAD), Panic Disorder (PD), Generalized Anxiety Disorder (GAD) and Post-Traumatic Stress Disorder (PTSD) sometimes prevent young people from attending school or adults from attending work, and in all those situations friends or family relationships may be seriously compromised. In the case of OCD peers or relatives may sometimes attempt to reduce the sufferer’s anxiety in participative actions in the compulsive rituals or in other cases, they may also exacerbate the anxiety by punishing the patient for his or her compulsive behaviour. In extreme cases, these compulsions can become so extreme that the affected person becomes constricted.
Epidemiology, Risk Factors and Course of Anxiety Disorders
Anxiety Disorders are the most common types of psychological disorders, and the lifetime prevalence rate in adults in the US National Comorbidity Survey Replication was 28.8% (Kessler et al., 2005). There is a consensus that Phobias are the most prevalent anxiety disorders and OCD is the least prevalent across a wide range of epidemiological studies (Kessler et al., 2009; Furr et al., 2009). For Phobias, lifetime prevalence estimates range from 6% to 12%, whereas those with OCD fall below 3%. Generalized Anxiety Disorder (GAD) has a lifetime prevalence of 1% to 6 %, whereas Panic Disorder in adults and Separation Anxiety in children range from 2% to 5%. In National representative samples, the prevalence of PTSD ranges from less than 1% or 2% in Western Europe to almost 8% in the US. The great variability is believed to be due to the fact that PTSD rates depend on the prevalence and traumatic exposure within specific locations geographically and the vulnerability of the populations within these countries to developing PTSD – in populations exposed to terrorism the prevalence is 12% – 16% (DiMaggio & Galea, 2006).
In people suffering from Anxiety Disorders, there is also a high risk of comorbidity [i.e. other anxiety disorders may also be present], and up to 1/3 of those suffering from Anxiety Disorders also suffer from another (Kessler et al., 2009) – they may also occur comorbidly with mood disorders in adults as well as children, substance use disorder in adults and adolescents and disruptive behaviour in young people/children (Furr et al., 2009; Huppert, 2009; Zahradnik & Stewart, 2009). In cases where substance misuse is also present, the use of drugs or alcohol is quite common in managing anxiety.
OCD is also present in a significant proportion of people with eating disorders such as anorexia nervosa. (Halmi, 2010).
We can observe a clear age and gender difference in the prevalence of Anxiety Disorders (Antony & Stein, 2009a; Furr et al., 2009; Kessler et al., 2009) and across most studies that are available, the modal age of the onset in Separation Anxiety Disorder and Specific Phobias is during the developmental phase in childhood [a stage pointed out by both great Western psychotherapists, Freud and Lacan, and also John Bowlby in his observational research on the development of attachment types in children at this critical stage of development], whereas that of anxiety disorders generally happens during adolescence or adulthood. In both adults and children, there is a tendency for more females to suffer from Anxiety Disorders than males, with the exception to this balance being for OCD which has a similar number men and women suffering from the condition although it is the rarest of anxiety disorders.
Anxiety Disorders tend to show a recurring episodic course with a gradual reduction in prevalence over the course of the life cycle (Kessler et al., 2009). It is also worthy to note that most children with anxiety disorders do not grow up to be adults with anxiety disorders or depression, however most anxious adults do have a history of childhood anxiety disorders. There are a number of risk factors associated with Anxiety Disorders and these include anxiety disorders or psychological disorders in the direct genetic network, an inhibited temperament of behaviour, neuroticism as a trait of personality, a personal experience of psychological problems, a history of over-controlling or critical parents, a history of conflict and violence and a history of stressful life events (Antony & Stein, 2009b; Pine & Klein, 2008). In the scenario of Anxiety Disorders, a behaviourally inhibited temperament is generally the tendency from birth – to become nervous and withdrawn from unfamiliar situations and stimuli. Neuroticism is a trait of personality that gradually develops over the life-span, and it is characterized by the tendency to escape negative affect and includes hostility, anxiety and depression in its manifestations.
In those suffering from Post-Traumatic Stress Disorder (PTSD) the additional factors that increases the risk for development include the severity of the trauma, high-life stress following the trauma, low socio-economic status, low support [from friends or those considered as friends], low intelligence and low educational level (Ehlers, 2009; Ozer et al., 2003). In PTSD, dissociative experiences tends to refer to abnormalities of perception, memory or identity such as derealisation [seeing the world as dream-like], depersonalization [seeing oneself from an external perspective or inability to recall important information]. In the case of parents with PTSD, their children are also at a higher risk of developing the disorder (Pine & Klein, 2008).
_____________________________________
Part 3 of 5 | Depression


Source: World Health Organisation
The states of being happy or sad are adaptive feelings, and many behaviours that lead to happiness among human beings, such as socializing [with the people that matter to the subject], becoming completely absorbed in productive work and developing longstanding friendships that are meaningful around values and loyalty, are important not only for the emancipation of the individual but also for a harmonious and functional society that embraces the “humane” qualities of mankind in all its creative aspects.
Sadness on the other hand is a psychological state commonly preceded by loss [of various kinds, which may range from material objects to valued relationships or abilities/skills and status related to them through accident or disease or other situations], and it is a negative feeling which may also be adaptive, in a sense that it is a reminder to most people [at least for those who are NOT philosophically oriented / cultured or have an understanding of values and loyalty in interpersonal relationships], that valued things or people need to be taken care of if they do not want to lose them in the future, especially the common volatile brain [i.e. the basic Darwinian instinct-guided average brain that lacks reflective abilities, reasoning skills, intuition and insight, while also failing to realises or understand the motivation behind its behaviour until matters have taken a disastrous course]. Sadness is also a way of signalling to others that we as human beings also need care and elicits [to most psychologically healthy human beings with a theory of mind] support that soothes our emotional pain – this is what makes us a superior breed of primates, i.e. our ability to reason and evolve with emotions as a propulsive form of energy for both individual and group, like Alexandre Dumas put it, “Un pour tous et tous pour un!” [French for “One for all and all for one!”].
Some extreme states of mood such as depression and mania are less adaptive than happiness and sadness; and it is now commonly known that during periods of hypomania or mania some patients suffering from Bipolar Disorder [which is characterized by episodes of mania and depression] produce highly creative artistic work (Silvia & Kaufman, 2010). This should not lead us to the conclusion that ALL creative people with extreme ways of exploring and expression their emotions through art suffer from Bipolar Disorder. But for those who do suffer from Bipolar Disorder and produce creative work, this highly valued asset comes at a price, since these individuals generally involve themselves in high-risk behaviours that come with the possibility of severe dehydration and exhaustion during manic episodes.
Seasonal Affective Disorder [or Winter Depression, its colloquial name] is a condition that is believed to be linked genetically to our cave-dwelling ancestors from the prehistoric era, who may have hibernated – an adaptive behaviour for the ancestors. However, in the world of today, depression does not seem to serve any adaptive function, and despite this, it remains a highly prevalent condition that affects up to 25% of the population (Kessler & Wang, 2009); because of this prevalence the main focus of this section will be on Major Depressive Disorder.

Share of the population reporting that they had chronic depression / Source: EuroStat
It is quite fundamental to grasp that depression is not simply “feeling sad”, as Major Depressive Disorder is an ongoing condition characterized by episodes of low mood and loss of interest in pleasurable activities along with other symptoms such as poor concentration, fatigue, pessimism, suicidal thoughts, and sleep and appetite disturbance. Depression is a serious public health concern because it radically decreases the quality of life of those affected, is a huge economic burden in terms of reduced productivity [and lack of creativity] among the national work force, and it also has adverse effects on the mental health and adjustment of the children of the depressed people (Garber, 2010; Kessler & Wang, 2009). This section will focus on the clinical features, epidemiology, risk factors and course of depression [suicidal risks will also be discussed].
Clinical Features of Depression
Severity
Depression can be classified as mild, moderate to severe, depending on the degree of impairment
Melancholia
In regards to somatic or melancholic features, in severe depression where there is a loss of pleasure in all activities [known as anhedonia] and a lack of reactivity to pleasant stimuli along with diurnal variation in mood and sleep and appetite disturbance, we tend to qualify such episodes as having melancholic features. Historically [please take note that this is not the case anymore], there was an ongoing view that these symptoms reflected “endogenous”, a genetically determined and biologically based form of depression, as different to a “reactive” depression arising from exposure to stressful life events and environmental adversity (Monroe et al., 2009).
However, the difference between these 2 forms of depression was not supported by empirical research, which instead shows that ALL episodes of depression are preceded by stressful life events, and that in any given scenario, we tend to have a combination of genetic vulnerability and environmental adversity that contribute to the development of depression (Parker, 2009).
Psychotic Depression
When mood disrupting delusions and hallucinations are present, depressive episodes are described as having psychotic features. Mood-congruent delusions are generally firmly held beliefs that are extremely pessimistic in nature and that have no basis in reality [illogical and cannot be explained and justified; for e.g. that a completely innocent individual is guilty of many wrongdoings and deserve to die. Mood-disrupting hallucinations in depression are generally auditory and sometimes involve the hearing of voices in a complete absence of any form of external stimuli [uncontrolled and unimagined and ongoing for months], which has negative advices to the sufferer [e.g. You are a failure, you are guilty of wrongdoing, or evil].
Among children, adolescents and adults, there has been a range of clinical features identified through both clinical observation and empirical research (e.g. Bech, 2009; Brent & Weersing, 2008; Gotlib & Hammen, 2009; Nolen-Hoeksema & Hilt, 2009a). Common clinical features of depression tend to affect the domains of cognition, perception, mood, somatic state, behaviour and relationships. Loss is once again a main thematic feature in depression as pointed out by Psychoanalytic Theories [loss of any kind, e.g. material, emotional, relationship, valued attribute due to sickness/accident, health, etc], and clinical features may be linked to those different domains of mental life.
Perception
In regards to perception, depressed individuals who have suffered some form of loss [internal or external] tend to perceive reality and the world as one where further losses are possible, and individuals who suffer from depression also selectively attend to negative stimuli and features in the environment. This leads them to engage in further depressive cognitive patterns in their thoughts processes and unrewarding behavioural patterns which amplify their depression’s severity – in cases of severe depression, mood-congruent auditory hallucinations are often reported. Hence, depressed people or people with depressive personality traits tend to come across as repulsive and despicable because of their obsessive disposition to only perceive the negative side of everything and every situation that life has to offer [note: this is different to constructive criticism which is normally for a purpose and comes with systematic reasons for enhancement]. Psychologists tend to go with the assumption that such severe perceptual abnormality is present only when patients report hearing harsh critical voices or containing depressive contents [as mentioned above]. These auditory hallucinations are also present in schizophrenia, however they are not always mood-congruent like in depression.
Cognition
Depressed patients tend to describe the world and the fabric of reality of their subjective experience in negative terms, this also include descriptions of themselves and their abilities [e.g. occupational and social accomplishments] – this negative evaluation is often portrayed as guilt for not living up to the standards [they set themselves based on their ‘perceived’ abilities] or for letting others down. They sometimes perceive their direct environments [peers, network, family, work colleagues or school/university] as hostile, apathetic, critical and unrewarding. The future is also described in very bleak terms by those suffering from depression, and they also report little if any hope that matters will improve. When extreme hopelessness is reported is it usually accompanied with excessive guilt for which the patients believe they should be punished – suicidal ideas and intentions may also be declared. In depressive delusional systems, extremely negative thoughts about the self are generally reported with the world and their future entangled in them.
Besides the content and thoughts being incredibly negative and bleak, depressed patients also tend to display concentration problems and logical errors in their thinking. These mistakes in reasoning are also characterized by a tendency to maximise the significance of negative events and minimize the significance of positive ones. Depressed patients also suffer from memory problems and struggle to remember happy events but instead have global over-general autobiographical memories about both positive and negative events. In addition to these, this category of patients also suffer from concentration, attention and decision-making problems that in turn give rise to difficulties managing leisure activities requiring sustained attention and academic or occupational responsibilities.
Affect
The impact on the patient’s affect tends to lead to low mood, and diurnal variations in mood and anhedonia. The depressed mood is usually reported as a feeling of sadness, loneliness, emptiness and despair. Diurnal variations in mood is usually quite common in severe cases of depression, with the patient’s mood generally being worse in the morning or after waking up. In cases of major depression, as a person moves from mild to moderate to severe depression, the increasing number of symptoms along with the intensity can also lead to intense anxiety. Generally, fears are experienced in the form of “Will this get worse? Am I stuck in this living hell forever? Will I ever be myself again? Will I be able to prevent myself from committing suicide to escape? Irritability is also a characteristics of depression, with the patient sometimes expressing their anger at the source of their loss [e.g. anger at a deceased one for abandoning the grieving person or sometimes at the health professional for not being able to alleviate their depressive symptoms].
Somatic State
The changes in the patient’s somatic state associated with depression include the disturbances of sleep and appetite, the loss of energy, failure to make age-appropriate physiological growth, weight loss, pain symptoms and a loss of interest in sexual activities. Commonly, depressed people struggle to find sleep and eat insufficiently due to their poor appetite; these symptoms are known as vegetative features. The sleep disturbances in depressed people generally involve problems trying to sleep, wakefulness at night or early-morning sleep disruption. Other symptoms such as racing thoughts and engaging in depressive rumination while unable to sleep is also quite common. In atypical cases of depression, patients may sometimes oversleep due to a constant feeling of exhaustion and consume excessive food due to an increased appetite or due to the feeling that eating may temporarily reduce their distress.
Medically unexplained chest, abdominal and back pain along with headaches are some of the additional features of depression. In some cases the pain symptoms are some of the first signs that would be reported to the doctor and it is only when the medical investigations of these symptoms turn out to be negative that depression is suspected to be the cause. All the somatic symptoms mentioned are consistent with research: dysregulation of neurobiological, endocrine and immune functions is associated with depression and the sleep is also affected.
Behaviour
Depressed patients are characterized behaviourally by the reduced and slow activity levels [psychomotor retardation] that they display, and are often helpless [without any control over their abilities] about their inability in getting involved in activities that could have helped their condition by bringing a sense of achievement or connectedness to meaningful [those chosen by the individual as a person with significance to him/her – note that it is a choice] people in their life. In rare cases some individual become house bound and immobile; such a condition is known as depressive stupor.
One of the major risks of depression is self-harm [a clear distinction is made between non-suicidal deliberate self-harm and suicidal behaviour]. In non-suicidal tendencies, patients may cut or burn themselves to distract themselves from the depressive feelings. In some cases, some have taken non-lethal overdoses to elicit attention and care from their close ones or to simply gain admission to hospital and remove them from the stressful situations that may have been amplifying their depressive symptoms.
Relationships
Depressed patients generally report a deterioration in their relationships with a range of significant figures in their lives from a wide range of environments [from professional to personal], and describe themselves as lonely, unable or unworthy to take steps to try and engage in some form of contact with others. Surprisingly, when the depressed attempt to overcome their loneliness by talking to others, they tend to come across as repulsive, unpleasant and draining through their depressive behaviour, pessimistic belief and sometimes arrogant narcissistic talks, this drives away those they interact with.
Video: Comment faire avec les gens frustrés ? – Benoit Zwick (2019)
Epidemiology, Risk Factors and Course of Depression
The most common mood disorder is Major Depression, and it has a lifetime prevalence rate of 6 – 25% in international community studies (Kessler & Wang, 2009). In the US National Co-morbidity Survey Replication the lifetime prevalence of DSM-IV Major Depression was 16.6% (Kessler et al., 2005). It is good to note that Depression is less common among pre-pubertal children than adolescents and adults (Brent & Weersing, 2008). Among children the number of boys to girl with depression is equal, however this changes in adolescence and by adulthood; compared with men, about twice as many women have depression (Nolen-Hoeksema & Hilt, 2009b).
In most cases of depression, there are many comorbid disorders also present. In the US, National Comorbidity Replication Survey, 59% of depressed patients suffered from comorbid anxiety disorders and 24% had comorbid substance use disorders (Kessler & Wang, 2009). Depression also tends to follow a chronic relapsing course, with up to 80% of people suffering from recurrent episodes, and it has been found that the median duration of episodes in community samples typically lasts for about 5-6 weeks. In clinical samples depressive episodes tend to last for about 5 to 6 months; the majority of cases however recover within 1 year and about half of patients continue to suffer from fluctuating residual symptoms between those depressive episodes; and for less than 10% of patients, recovery does not occur and chronic depressive symptoms persist and most cases relapse within 5 years (Angst, 2009; Boland & Keller, 2009).
During treatment, as more depressive episodes occur, we tend to notice a decrease in inter-episode intervals and a reduction in the amount of stress required to trigger the onset of further depressive episodes, an issue related to Stress Theories (Boland & Keller, 2009).
NOTE: Stress theories propose that individuals develop depression following exposure to stress. The diathesis- stress theories propose that depression only follows after exposure to stress in people who have specific biological or psychological attributes that render them more vulnerable to stressful life events, and the most vulnerable require the least stress to trigger depression (e,g., Joiner & Timmons, 2009: Joormann, 2009; Levinson, 2009). On the other hand, Stress-generation theory proposes that people with certain personal attributes inadvertently generate excessive stress, which in turn leads to depression (Liu & Alloy, 2010)
The risk factors for depression include a family history of mood disorders, female gender, low socio-economic status involving educational and economic disadvantage, and adverse early family or institutional environment, the depressive temperament, a negative cognitive style, deficits and self-regulation, high levels of life stress, and low levels of support from meaningful others (Garber, 2010; Hammen et al., 2010).
Risk factors for recurrent major depressive episodes identified in the US collaborative depression study of 500 patients, include a history of three or more prior episodes, comorbid dysthymia (often known as Double Depression), comorbid anxiety and substance use disorders, long duration of individual episodes, poor control of symptoms by antidepressant medication, onset after 60 years of age, the family history of mood disorder, and being a single female (Boland & Keller, 2009).
Four small category of people who suffer from depression, deficits the visual processing of light and the season of the year are risk factors for depression (Rosenthal, 2009). These people, who experience regularly recurring depressive episodes in the autumn and winter, with remission in the spring and summer, are generally considered as suffering from Seasonal Affective Disorder. These patients develop symptoms in the absence of adequate light and respond positively to enhanced environmental lighting, often referred to as “Light Therapy or Treatment” (Golden et al., 2005).
In community samples about 3.4% of people with major depressive disorder commit suicide; the rate in clinical samples about 15%; about 60% of completed suicides (studied by psychological autopsy) had suffered from depression (Berman, 2009).
_____________________________________
Part 4 of 5 | Schizophrenia

Before covering the topic of schizophrenia, it is important to take note that the condition is commonly confused to refer to another condition that involves split-personalities, and this is mostly a trend that lives in the world of pop culture and Hollywood. About 40% in the UK equated split or multiple-personality with schizophrenia in a National Survey (Luty et al., 2006). However, after covering this section, we hope that the confusion will be cleared since schizophrenia does not refer to conditions that involve split-personalities [the closest scientific equivalent to this state of being, is a condition known as Multiple Personality Disorder or Dissociative Identity Disorder and are both not as debilitating as schizophrenia with treatment being much more effective].
Schizophrenia refers to a collection of seriously debilitating conditions characterised by positive and negative symptoms in this organisation (Mueser & Jeste, 2008).
Delusions and hallucinations are the principal positive symptoms of schizophrenia. Delusions are strongly held, unfounded, culturally alien beliefs. For example with persecutory delusions, individuals may believe that a group of people conspiring to harm them [this should not lead us to believe that a healthy person with a suspicion caused by the critical analysis of a person or group of people is deluded and is schizophrenic – remember that human beings have individual personalities too]. Hallucinations on the other hand involve experiencing sensations in the absence of external stimuli [e.g. with auditory hallucinations – which are the most common type in schizophrenia – people reported hearing voices that others cannot hear].
The negative symptoms of schizophrenia include flattened affect, alogia and avolition. In the case of flattened affect, the emotional expression of the patient is limited, and with alogia there is an impoverished thought that is inferred from the patient’s speech. Short brief and concrete replies are given to question [this is referred to as poverty of speech], or in some cases speech production is normal but it conveys little meaning and information due to repetition, or being overly abstract [referred to as poverty of content], or being too concrete. When patients suffer from avolition, a lack of goal directed behaviour can be observed. The negative symptoms generally give rise to a restricted lifestyle involving little activity, little social interaction with others and little emotional expression – disorganisation may also affect both speech and behaviour [disorganised, illogical, incoherent, speak are the signs of an underlying formal thought disorder]. Disorganised catatonic behaviour is usually characterised by the complete absence of spontaneous activity or excessive purposeless activity.
Schizophrenia is a debilitating and re-occurring condition that comprises the capacity to carry out normal activities, and also consists of incomplete remission between episodes. (Hafner & der Heiden, 2008). Symptoms of schizophrenia typically appear in late adolescence or early adulthood, wax and wane over the life course, and have a profound long-term effect on patients and sometimes their families.
Schizophrenia is considered to be the most debilitating of all psychological disorders, since it affects the patient’s capacity to live independently, make and maintain satisfying and enduring relationships, engage in family life, parent children effectively, work productively and enjoy leisure activities. Rates of unemployment, homelessness and imprisonment are very high among people with schizophrenia, although just under 1% of people suffer from schizophrenia, the World Health Organization has rented as second only to cardiovascular disease in terms of overall disease burden internationally (Murray & Lopez, 1996).
Despite these unattractive facts, the scientific advances in our understanding of schizophrenia, along with advances in both psychological and pharmacological approaches to treatment, making it increasingly realistic for people who suffer from schizophrenia to live far more productive lives than were previously possible (Mueser & Jeste, 2008).
Case Example of Schizophrenia
A young man, named Julian was referred for assessment and advice by his doctor. Since returning to his rural home after studying in London for one year, his parents started to worry about his state because of his strange behaviour. After failing as exams, the patient said that he had to ”sort his head out”. Since his return, the parents had noticed a lack of concentration along with incoherent speech during his conversations which happen most of the time – his behaviour was also erratic and unpredictable.
The parents concern grew when Julian suddenly went missing a few weeks prior to the referral. After hours of searching, he was found about 55 Km from their home, dehydrated, exhausted and dressed only in sport shorts, singlet and running shoe. After enquiry, the latter developed the belief that a secret mission in the East had to be undertaken by him; and as he started jogging in the morning, he headed eastwards towards the rising Sun. He even planned to jump onto the car ferry when he reached the coast, across the sea over to Holland, and continue east towards India in his secret mission [reminiscent of a James Bond episode].
Since the episode, Julian has spent much of the time in his room muttering to himself, often becoming quite distressed, and when his parents spoke to him they found it hard to make any sense out of his words.
Family History
Julian was the 19-year-old son of a prominent farmer in a rural English village where the whole family lived in a large amount on an extensive estate. The farm was managed by the patient’s father; who had a traditional authoritarian manner and a positive, if distant, relationship with Julian. While he was incredibly worried about Julian and to the search for him, once the latter was found, the father returned to work unless the care of his son to his wife.
The mother was an artist who dressed flamboyantly, behaved in a theatrical manner and held century, unconventional beliefs [e.g. Conspiracy theories about many issues, was interested in eastern mysticism and believe that faith healing and alternative medicine were preferable to traditional Western medicine]. These characteristics of a personality along with her beliefs affected her treatment of Julian after the ”Running East” episode, where she engaged the latter in intense conversations about mystical meaning of the psychotic experiences that led to him trying to make his way to India on foot. Rather than taking Julian to the accident and emergency department of the local hospital for assessment, she brought him to a feeler and then than homeopathist. It was only of these interventions failed to our view the distress that she took Julian to the doctor, who made the referral to the community mental health team. In the preliminary assessment that was conducted with Julian and both of his parents, the mother responded to the son with intense emotional over involvement (an index of high expressed emotion associated with a relapse in schizophrenia; Hooley, 2007).
With regard to the extended family, according to parents there has never been a family history of psychological disorder. However some members of the mother’s well-to-do family were fairly eccentric and odd, especially her brother, Sedric, and her uncle, William Jr. Williams eccentricities led him into serious conflict with his father, and Sedrick’s odd behaviour underpin his highly conflictual, childless marriage.
Developmental history
Julian on a family farm and went to the local school, his development was what most people would call normal. His Academy former school was above average and he had many friends in his local village, and was a popular child and adolescent who also excelled at cricket. At 18 years old before going to university London, he had no psychological problems.
His first term at college was successful academically and socially, however, the occasional experimental cannabis use that had begun the summer before going to college turn to a regular use once Julian moved to London. During his time at university, the patient also experimented with LSD on a few occasions. In the final term of his first year at college, Julian developed intense fear of exam failure. Other symptoms quickly followed such as difficulty studying effectively and sleeping problems. Julian stopped attending classes regularly and spend more time alone, and was relieved to return home after sitting as exams. Once home he was described as quiet and thought during most of the time prior to the “running East” episode.
Presentation
Julian presented with symptoms such as delusions, hallucinations, disorganised speech and anxiety. At the very start the patient was very reluctant to be interviewed because he believed he had urgent business to attend to in Holland and further afield in India. He also showed signs of being anxiously distressed throughout the interview, explaining that his path was to the east and believed he was being called there by an unknown source. He firmly believes this because of a sign he had seen while out jogging on the morning of the enigmatic “running East” episode. The way in our God will record the sunlight and cast a shadow on the red barn against which it was leaned made a distinctive pattern, which to him meant a special sign indicating that he should go East, first to Holland and then all the way to India. Upon questioning this idea, a clear authoritative voice said that he should leave at once.
At this point in his narrative, stopped mid-sentence and displayed thought blocking, and will strive the topic he was talking about. Upon being asked to continue his story, he began to giggle, and when questioned about the reason behind his amusement, Julian declared to have heard someone say something funny. Julian then spoke about a number of unrelated topics in an incoherent way before experiencing thought blocking again.
Later he expressed the desire to leave soon because people will try to prevent him, as he had heard them plotting about this the day before, and also declare that they had tried to put bad ideas into his head [which he described as frightening]. He was also frightened by periodic sensations that everything was too loud or too bright and coming at him, declaring “it was like doing acid [LSD] all the time… a really bad trip.”
Formulation
In Julian’s case he presented with auditory hallucinations, delusions, thought disorder, anxiety and a significant deterioration in social and occupational functioning which had been present for more than 1 month [symptoms consistent at the time of this essay with a diagnosis of Schizophrenia]. The patient also showed a complete lack of insight and was unable to understand that the voices being heard were hallucinations and that the delusional beliefs were unfounded. Among the major precipitating factors were the experience of recent exam pressure and his transition from living at home to living in London at attending college. The principal predisposing factors were possible genetic vulnerability to psychosis and a history of hallucinogenic drug use.
His psychological condition was maintained by what was likely to be an excessive level of maternal expressed emotion characterised mainly by emotional over-involvement. His delusions were also reinforced by the mother since the latter engaged Julian in long and draining conversations about them. The protective factors in this case were godo premorbid adjustment and a strong family support for the boy.
Treatment
The treatment plan included antipsychotic medication and family will to reduce parental expressed emotion, with an initial brief period of hospitalisation. Julian did recover from his first psychotic episode, and his hallucinations and delusions decrease considerably with medication. Through family Psycho-education, parents develop understanding of this condition and of the requirement of a “low-key” approach to interacting with the boy as he recovered.
However some obstacles were encountered in Julian’s recovery, since he disliked the side effects of the medication, especially the weight gain and reduced sexual drive/function, and so had poor medication adherence – depression also manifested during the remission, when Julian came to realise about the many losses that followed his condition. He was unable to pursue his university studies and thus, could not continue the law career he had dreamed of. He also experienced difficulties in maintaining friendships or to commit to engaging on a regular basis in physical exercises or sports. When his mood was low, Julian would smoke some cannabis to lift his spirits.
The mother found it very difficult to accept the diagnosis of Schizophrenia and continued to hold the belief that his psychotic symptoms were linked to some spiritual or mystical explanation. She even sometimes declared that she thought of her son not as an ill young man, but a gifted seer or a “chosen one” [based on no rational explanation or series of events], and often engaged Julian in intense, distressing conversations about these issues. In the years that followed his initial assessment, poor medication adherence, ongoing cannabis use [which the patient could not tolerate unlike some other users] and exposure to high levels of intrusive parental emotions led Julian to relapse more often than might otherwise have been the case.
Clinical Features of Schizophrenia
A range of clinical features have been identified and associated with Schizophrenia though research and clinical observations (Mueser & Jeste, 2008). The generally concern the domains of perception, cognition, emotion, behaviour, social adjustment and somatic state.
Perception
At the perceptual level, patients suffering with schizophrenia generally describe a breakdown in perceptual selectivity, with difficulties focusing on essential information or stimuli to the exclusion of accidental details or background noise. Most aspects of the environment seem to be salient, however, the inability to distinguish between figure and ground is a serious problem to the sufferer. During an acute psychotic state, internal stimuli such as verbal thoughts are experienced as auditory hallucinations that have the same sensory quality of the spoken word.
Auditory hallucinations can sometimes be experience as extremely loud thoughts, or as thoughts being repeated by another person aloud (thought echo), as voices speaking inside the head or as voices coming from somewhere in the outer environment. The auditory hallucination may occur as third person making comments on the patient’s action, as a voice speaking in the second person directly to the person, or as two or more people talking or arguing – the effect did may also perceive voices to vary along the number of dementia [may be construed as benign or malevolent, controlling or impotent, or knowing or knowing little about the patient, who may sometimes feel compelled to the demands of the voice or not.
When hallucinations are perceived to be malevolent, controlling, all-knowing, where the individual affected feels compelled to obey the demands of the voice, the situation is deemed to be far more distressing than those who do not have these attributes. While auditory hallucinations are the most common features in schizophrenia, hallucinations may okay other sensory modalities too. Somatic hallucinations also often occur in schizophrenia, with many cases including reports of electricity in the body or the feeling of something crawling underneath the skin [these may be qualified as delusional interpretations. For example, a patient reported that the television was activating a transmitter in her pelvis and she could feel the electricity from this closing insects to grow and move around under the skin. Visual hallucinations [seeing visions] are relatively rare in schizophrenia very common in temporal lobe epilepsy.
Cognition
At the cognitive level, delusions are the most common cognitive clinical feature of schizophrenia, and are false, idiosyncratic, illogical and stubbornly maintained erroneous inferences drawn to explain unusual experiences, such as hallucination. [e.g. patient with auditory hallucinations where an authoritative voice commanding the latter to gather the children, was interpreted by the patient that she had been chosen by God to prepare all the children for the second coming of Christ]
Delusions may also arise from unusual feelings associated with psychosis. Persecutory delusions may develop from feelings of being watched. Delusions of thought insertion or thought withdrawal may develop as explanations for feelings that thoughts are not one’s own, or that one’s thoughts have suddenly disappeared. Factor analyses show that delusions fall into 3 broad categories:
Delusions of influence [including thought withdrawal or insertion, and beliefs about being controlled]; delusions of self-significance [including delusions of grandeur or guilt]; and delusions of persecution (Vahia & Cohen, 2008). Delusions may vary in the degree of conviction with which they are held [great certainty to little servant, the degree to which the person is preoccupied with them [the amount of time spent thinking about the belief], the amount of distress they cause.
Particular sets of the may comprise of a confused sense of self, particularly paranoid delusions with the patient holds the belief that they are being persecuted or punished for misdeeds, or delusions of control where there is a belief that their actions controlled by others [e.g. an unknown source or entity].
A lack of insight along with an impaired judgement is quite common during a psychotic episode. This happens when the patient believes that the contents of their hallucinations and delusions are real, and are incapable of coming to terms with the fact that their experiences and beliefs arise from a clinical condition. However in between psychotic episodes, the patient’s insight may improve and in some cases they may acknowledge that their hallucinations and delusions are symptoms of schizophrenia.
Speech in schizophrenic patients is also fairly hard to understand due to the abnormalities in the underlying thought pattern. This formal thought disorder is characterised by
- Tangentiality [answers given to questions are off the point]
- Derailment [sentences makes sense but hardly any meaning is conveyed by the sequences of sentences because there is a constant jumping from one topic to another, with very loose association between topics and little logic to what is said]
- Incoherence [sentences are incorrectly formed so little sense can be made out of them]
- Thought blocking [the patient abruptly stop’s in mid-sentence and is unable to complete the train of thought]
- Loss of goal [the difficulty in following a logical train of thought from A to B]
- Neologisms [inexistent new words are made up that only have idiosyncratic meaning for the patient]
Cognitive impairment or deterioration occurs in schizophrenia and this may either be general or specific. In cases with general cognitive deterioration, we can observe a reduction in overall IQ with many cognitive function also negatively affected. With specific cognitive impairment one or more of the following functions may be impaired: attention, memory, cognitive flexibility, social cognition and executive function, and most commonly the ability and dedication to follow through on a planned course of action. Cognitive impairment remains a better predictor of disability and vocational functioning than positive symptoms.
Emotions
At the emotional level, especially during the prodromal phase, before an acute psychotic episode, anxiety or depression may occur in response to changes in perceptual selectivity and cognitive inefficiency. One of the main functions of relapse prevention is for patients to learn [and eventually master] the ability to identify and manage prodromal changes in affect.
During psychotic episodes that are intense, anxiety or depression may occur in response to hallucinations, delusions, formal thought disorder and other debilitating symptoms. Inappropriate affect may also be present in hebephrenic schizophrenia, where the patient responds to the internal stimuli such as auditory hallucinations [e.g. laughing wildly] and not the external social context. In chronic cases, blunted or flattened affect can also be observed, and in remission [following an episode of psychosis], the sense of loss [e.g. of valued personal relationships, material, career, etc] that comes with increased insight into the reality of the condition may give rise to post-psychotic depression in some cases.
Behaviour
In terms of behaviour, prodromal excitation may occur prior to an acute psychotic episode, characterised by sleep disturbance, impulsive behaviour, and over-reactivity [may include compulsive behaviour]. Avolition also occurs during psychotic episodes with an observable impairment in goal-directed behaviour.
In some chronic cases, it is common to also find catatonic behaviour along with an impairment in the ability to initiate and organise voluntary movement and posture. Catatonia may be either retarded or excited. Excessive purposeless motor activity is the hallmark of excited catatonia and may include stereotypies [repetitive actions], echolalia [repeating the words said by others] or echopraxia [imitating the actions of others] – these tend to occur without the patient being consciously aware of it [not a conscious choice]. In cases where retarded catatonic behaviour is present there is an observable reduction in purposeful activity; patients may display signs of immobility, mutism, adopt odd postures for extended amounts of time, and display waxy flexibility or negativism.
Social Adjustment
A marked deterioration in social adjustment is also common in schizophrenia, and the ability for self-care, appropriate dressing, grooming and personal hygiene deteriorates – patients with schizophrenia often look dishevelled and unkempt. A decline in also commonly present in the domains of education and work with a withdrawal from regular patterns of socialisation and difficulty making and maintaining significant relationships. A deterioration with others also occurs and schizophrenia tends to have a negative impact on parent-child, marital and sibling relationships.
Somatic State
Approximately 50% of people with Schizophrenia also have comorbid substance use disorders and almost 75% have significant health problems, with the most common one being Chronic Obstructive Pulmonary Disease (COPD) [usually due to heavy smoking]; heart disease and diabetes due to obesity; HIV/AIDS and hepatitis B and C caused by unsafe sex and intravenous drug use [e.g. heroin]. These drug and medical problems in schizophrenia are lifestyle problems. However, one the positive side, schizophrenia is associated with reduced rates of cancer and rheumatoid arthritis (Tandon et al., 2008a).
Epidemiology, Course, Outcome and Risk Factors of Schizophrenia
International epidemiological studies that have been reviewed have allowed for a number of conclusions to be deduced regarding schizophrenia. We know that [luckily] under 1% of the population suffer from schizophrenia, and the lifetime risk of the condition is about 0.7% (Saha et al., 2005). More men than women suffer from schizophrenia: the male-female ratio is about 1.4:1 (McGrath et al., 2004). Schizophrenia has an earlier onset in males (20-28 years) than in females (28-32 years) (Murray & Van Os, 1998). The rates for schizophrenia have also been found to be similar across countries and cultures when diagnostic criteria are used (Mueser & Duva, 2011).
Schizophrenia tends to follow a distinctive course although a considerable variability exists across cases (Jablensky, 2009; Jobe & Harrow, 2010; Mueser & Duva, 2011, Tandon et al., 2009). The onset of schizophrenia generally occurs in late adolescence or early adulthood and may be acute or insidious [onset generally takes place over 5 years, starting with negative and depressive symptoms, followed by cognitive and social impairment and finally positive symptoms]. Longitudinal studies suggest that there is an early deterioration phase that extends over 5-10 years, a stabilisation phase and a final gradual improvement phase. In over 50 – 70% of cases, the condition follows a chronic relapsing course, typically with incomplete remission between episodes. However, up to 40% of patients show one or more periods of complete recovery with good adjustment for at least 1 year, and 4 – 20% of cases show complete remission.
Psychotic episodes may last from 1 – 6 months, although some cases extend up to 1 year. They are usually preceded by a prodromal period of a number of weeks. Psychotic episodes may be lessened and the severity of the symptoms ameliorated through early detection and the use of pharmacological and psychological treatment. Inter-episode functioning may differ greatly and better inter-episode functioning is associated with a better prognosis. The duration of remission between episodes may be lengthened through the use of maintenance medication and psychosocial interventions to reduce stress and improve coping and illness management.
With treatment, usually positive symptoms (hallucinations and delusions) abate between episodes but negative symptoms (blunted affect, alogia and avolition) can be enduring and are more likely to persist during remission. In the stabilisation phase of schizophrenia, positive symptoms become less prominent, while negative symptoms and cognitive deficits become more prominent. The lifespan of people with schizophrenia is also 9 years less than that of the general population, and this is partly accounted for by the high rate of suicide during the first 10 years of the disorder and the high rate of comorbid medical disorders that also tend to occur along with schizophrenia. About 50% of schizophrenics attempt suicide or self-harm, and about 10% commit suicide (Heisel, 2008; Schennach-Wolff et al., 2011).
One of the greatest risk factors for schizophrenia is a family history of psychosis. Other risk factors make a small contribution to the overall risk within the context of associated with genetic vulnerability. However until now, it is important to note that we still do not have any clear consensus or evidence on how these risk factors operate and whether environmental factors remain a stronger prediction of the onset of schizophrenia than genetic factors that only set a predisposition [risk] of possibly developing the condition. Prenatal and perinatal risk factors, such as maternal flu infection and obstetric complications, are likely to have a negative effect or indirect effect on the development of the nervous system in line with the neurodevelopmental hypothesis that states how those affected by such issues while also being genetically predisposed to schizophrenia are even more neurologically vulnerable to psychosis (Murray & Lewis, 1987). Trauma exposure and most demographic risk factors (being unmarried, low-SES urban migrant) are associated with higher levels of stress and lower levels of social support [which increases the risk of psychosis in the genetically vulnerable] according to the Diathesis-Stress Conceptualisation of Schizophrenia (Zubin & Spring, 1977).
In the short term, relapse is more likely in cases where these is heavy cannabis use [along with poor personal/subjective tolerance of the effects on consciousness], poor treatment adherence, frequent contact with insignificant extended family members who may display excessive negative emotional expressions towards the patient [e.g. criticism, hostility and emotional over-involvement] and exposure to acute stress life events (Jablensky, 2009).
A poor outcome is associated with substance use and a longer period of untreated psychosis in people who have poor premorbid adjustment and an early insidious onset with no clear stressful life event preceding their first treated episode. One of the main traits associated with a poor outcome is “Anxiety”, and people with this stress profile are generally more sensitive to and reactive to life’s stressful events, along with populations living in a developing economy, and family-based stress associated with excessive negative expressions of emotion. The symptom profile predictive of a poor outcome is also marked by severe negative symptoms, cognitive impairment and lack of depressive symptoms.
A favourable outcome in schizophrenia is associated with a range of factors (Bota et al., 2011). These include good premorbid adjustment, and a brief duration of untreated psychosis characterised by an acute onset in response to precipitating stressful life events. A family history of affective problems/disorders [rather than schizophrenia] or little psychopathology and a personal symptom profile in which there are affective as well as psychotic features are also predictive of a good prognosis. A better outcome tends to follow those who have a favourable life situation to return to following discharge from hospital.
_____________________________________
Part 5 of 5 | The Effectiveness of Psychotherapy

The main help that a psychotherapist provides is psychotherapy, a contractual process where professionals with expert knowledge interact with clients to guide and help them in the resolution of their psychological conflicts, emotional imbalance, psychological problems and address mental health and behavioural difficulties [if any]. Psychotherapy can be offered to both adults and children on an individual, couple, family or group basis.
Often psychotherapists offer therapy as one element of a multimodal programme provided by a multidisciplinary team [e.g. a multidisciplinary adult mental health team may routinely offer a multimodal programme of psychotherapy combined with some mild anti-depressant for depression]. This final section will focus on the evidence base for the overall effectiveness of psychotherapy.
Evidence-based Practice
In today’s trend of mainstream clinical psychology where the mechanical model of early behaviourists has been combined with cognitive psychology to become Cognitive-Behavioural Psychology, there has been a gradual shift from practice guided by descriptions of clinical cases [qualitative, detailed and individual] to “evidence-based” practice guided by the results of empirical studies using the statistical methods of science to make inferences about behaviour [that can be measured at least] on the effectiveness of psychological interventions. This movement has started in part due to the influence of policies derived from the medical field which bases itself on evidence-based medicine [i.e. tested with laboratory-rigour and statistical methodology] (Sackett et al., 1996, 2000).
Evidence practice in medicine as it has been applied to psychology [or should we say behavioural science] involves the judicious and compassionate use of the best available evidence to make decisions about patient or client care. In clinical psychology, this involves considering available scientific evidence about “what works” on one side, and the client’s unique problems, needs, rights and preferences on the other; while also making balanced, compassionate judgements (APA Presidential Task Force on Evidence Based Practice, 2006; Norcross et al., 2006).
Meta-analyses
The most persuasive form of evidence as far as the effectiveness of psychotherapy and other psychological interventions are concerned in regards to empirical measurements and statistical methodology, comes from meta-analyses on controlled trials.
Meta-analysis is a systematic, quantitative approach to reviewing evidence from multiple trials while also reducing the impact of reviewer bias since the data from many trials are synthesised using statistical methods.
In a meta-analysis, effect sizes are calculated for each trial and then averaged across all trials to provide a quantitative index of the effectiveness of a particular form of treatment with a specified population. The effect sizes calculated in meta-analyses express quantitatively the degree to which treated groups improve over untreated control groups [A graphic explanation of the calculation of an effect size in given in FIGURE A.
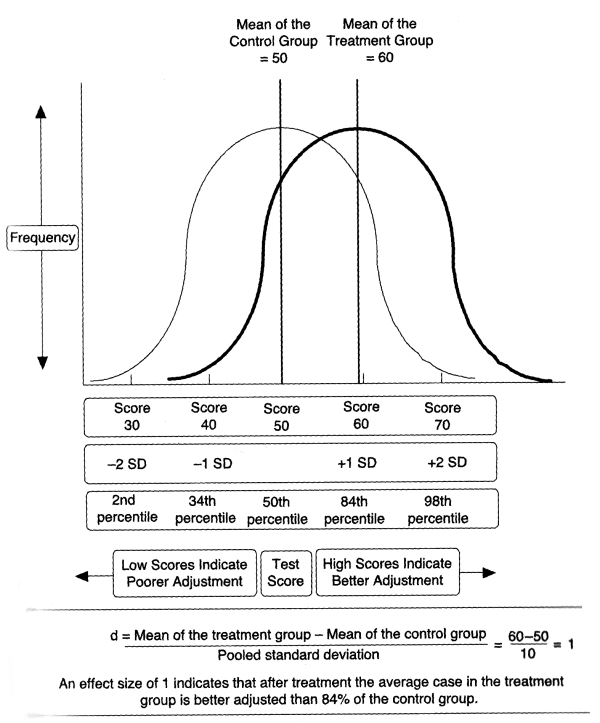
FIGURE A. A Graphic Representation of an Effect Size of 1
Table A shows a system for interpreting effect sizes, and using it, it may be seen that .9 is a large effect size, and if such an effect size was obtained in a meta-analysis it would mean that the average treated case fared better than 82% of the cases in the control group. It would also indicate that 71% of cases in the treatment group had a successful outcome compared with 29% of control group cases. Finally, a large effect of .9 would indicate that 17% of the variance in outcome would validly be attributed to the effects of the treatment rather than other factors.

TABLE A / Note: Adapted from Wampold (2001, p. 53). 1. From Cohen (1988), 2. From Glass (1976). 3. From Rosenthal and Rubin (1982). Binomial effect size display, assuming overall success rate of .5, success rate for treated cases is .5+ correlation with outcome/2, and success rate for untreated cases is .5-correlation with outcome/2. 4. From Rosenthal (1994, p. 239), percentage of variance = d²/(d² +4).
Is Psychotherapy effective? If so, how effective?
Mary Smith and Gene Glass published the first major meta-analysis of psychotherapy result studies in American Psychologist in 1977. They included 375 controlled trials of psychotherapy in their analysis and found an average effect size of .68. They concluded that a typical therapy client was better off that 75% of untreated individuals.
Since that seminal study many meta-analyses have been conducted, and in a synthesis of 68 separate meta-analyses of psychotherapy with children, adolescents and adults with a wide range of different psychological problems, Grissom (1996) found an aggregate effect of .75, indicating that the average treated case fared better than 77% of untreated controls.
Effects of Psychotherapy with Adults
The mentioned meta-analysis conducted by Smith and Glass (1977) also included many studies of therapy with children and young people. In the quest to determining the effects of psychotherapy for adults with psychological problems, Shapiro and Shapiro (1982) conducted a meta-analysis of 143 studies of psychotherapy exclusively involving adult populations. This revealed an effect size of 1.03, meaning that after treatment the average adult who participated in psychotherapy fared better than 84% of untreated control group cases.
Effectiveness of Psychotherapy with Children and Adolescents
The results of 4 broad meta-analyses of studies involving children and adolescents under 18 years with a diverse range of psychological problems receiving a variety of forms of psychotherapy provide evidence for the overall effectiveness of psychotherapy with children (Casey & Berman, 1985; Kazdin et al., 1990; Weisz et al., 1987, 1995). These meta-analyses included more than 350 treatment outcome studies. Effect sizes ranged from .71 to .88, with a mean effect size of .77. This indicates that the average treated case fared better than 78% of control group cases.
Psychodynamic Psychotherapy
Within the psychodynamic tradition, a distinction is made between short-term psychodynamic psychotherapy and intensive long-term psychoanalysis. Short-term psychodynamic psychotherapy involve weekly sessions for periods of 6 – 12 months, while Long-term psychoanalysis involves two or more sessions per week, usually lasting for periods longer than 1 year [Jacques Lacan, one of the main psychoanalytic figures in France, broke from other associations to create his own school where he advocated short psychoanalytic sessions that varied ranging from 10 minutes to more, as he argued that the point of therapy is to shape the patient’s consciousness and depending on the person, this can be achieved by a range of ways, e.g. metaphors or word plays that allows the patient to peer into his own psyche and understand himself]
Two important broad meta-analyses have been conducted to evaluate the effectiveness of psychodynamic psychotherapy with adult mental health problems (Leichsenring et al., 2004; Leichsenring & Rabung, 2011). In a meta-analysis of 17 studies, Leichsenring et al. (2004) found that short-term psychodynamic psychotherapy yielded an effect size of .7 for psychiatric symptoms in patients mainly diagnosed with anxiety and mood disorders when therapy was compared with waiting list or minimal intervention control groups. This indicates that after treatment the average treated case fared better than 76% of controls. In this meta-analysis, the outcome for psychodynamic psychotherapy did not differ from that of other forms of psychotherapy in the 14 studies where such comparisons were made.
In a further meta-analysis of 10 studies, Leichsenring and Rabung (2011) found that Long-term psychodynamic psychotherapy involving more than 50 sessions over periods longer than a year yielded an effect size of .54 for overall effectiveness for complex cases with severe symptomatology, comorbid diagnoses, or personality disorders, when long-term psychodynamic psychotherapy was compared with a range of other therapies including Cognitive-Behavioural Therapy (CBT), dialectical behaviour therapy, family therapy and short-term psychodynamic psychotherapy. This indicates that after treatment the average case fared better than 70% of cases treated with other therapies. The gains made during treatment were sustained at 1 to 8 years after follow up.
The results of these two meta-analyses show that short-term psychodynamic psychotherapy is an effective as other widely used forms of psychotherapy, including Cognitive-Behavioural Therapy (CBT), for common psychological problems such as anxiety and depression in adults; and that long-term psychodynamic psychotherapy is more effective that some other forms of therapy for adults with complex mental health difficulties.
Client-centred Humanistic Psychotherapy
Elliot et al., (2004) conducted a meta-analysis of trials of psychotherapy that fall broadly within the client-centred humanistic psychotherapy tradition [over 90 trials of client-centred, experiential, gestalt and emotionally-focussed therapy were included in the analysis]. Clients in these studies had a wide variety of psychological problems including anxiety, mood, eating and relationship distress. The average duration of treatment was 22 sessions, reflecting about 6 months of therapy. An effect size of .78 was obtained, indicating that the average treated case fared better than 78% of cases in control groups. These results indicate that client-centred humanistic psychotherapy is an effective form of treatment for a range of common psychological problems in adulthood.
Overall Effects of Psychotherapy
FIGURE B summarises the results of meta-analyses, described above, of the effectiveness of psychotherapy from a range of different traditions with adults and children. In this figure, where appropriate, effect sizes from multiple meta-analyses have been averaged, and graphed as success rates based on the system given in TABLE A.
From FIGURE B it can be deduced that meta-analyses of psychotherapy trials yield moderate to large effect sizes that range from .65 to 1.02. When expressed as success rates, the results of meta-analyses indicate that 65 – 72% of people with psychological problems benefit from psychotherapy. Thus approximately two-thirds to three-quarters of people who engage in psychotherapy find that it leads to improvements in their mental health.

FIGURE B. Success Rates of Psychotherapy with adults and children, and Therapy from other schools of thought [traditions] based on Effect Sizes from Meta-analyses
In order to make sense of the overall effectiveness of psychotherapy, it may be useful to ask ourselves: Are the moderate to large effect sizes associated with psychotherapy very different from those associated with the medical and surgical treatment of physical illnesses, diseases and medical symptoms?
In a synthesis of 91 meta-analyses of various medical and surgical treatments for a range of medical conditions, Caspi (2004) found an average effect size of .5. This falls in the moderate range of effect sizes (.5 – .8) and not very dissimilar to the effect size of .75 from Grissom’s (1996) synthesis of 68 meta-analyses of psychotherapy trials mentioned at the beginning of this section. Hence, it may be concluded with some certainty that the moderate effect sizes associated with psychotherapy are similar to those associated with the treatment of medical conditions.
Deterioration and Drop-Out
A consistent finding within psychotherapy research literature is that up to 10% of clients deteriorate following treatment (Lambert and Ogles, 2004; Lilienfeld, 2007). In a review of 46 studies on negative outcome in adult psychotherapy, Mohr (1995) found that deterioration was associated with particular client and therapist characteristics and particular features of psychotherapy. Deterioration was much more common among clients with obsessive compulsive disorder or severe interpersonal difficulties. Lack of motivation and the expectation of benefiting from psychotherapy without personal effort were also associated with deterioration. Deterioration was more common when unskilled therapists lacked the empathy and did not collaborate with clients in pursuing their agreed goals. Failure to manage counter transference appropriately and frequent transference interpretations were also associated with deterioration.
Dropping out of psychotherapy is a relatively common event. In a meta-analysis of 125 studies, Wierzbicki and Pekarik (1993) found a mean dropout rate of 47%. Dropout rates were higher for minority ethnic groups, less educated clients, and those with lower incomes. Thus, we can conclude that about 1 in 10 clients deteriorate following therapy and that marginalised clients with particularly troublesome disorders and negative attitudes to psychotherapy are vulnerable to dropping out of psychotherapy and deterioration.
Medical Cost Offset
So, all the evidence that has been reviewed shows that psychotherapy is effective for a range of problems and populations. However, an important factor regarding the delivery of psychological treatment is the financial implication of it [i.e. the cost to the economy and health services]: How much does it cost to provide such a psychotherapy service? From this financial perspective, two questions would be of interest:
First: Do clients who received psychotherapy use fewer medical services and so incur reduced medical costs? This saving would be referred to as the Medical Cost Offset.
Second: Is the Medical Cost Offset associated with psychotherapy greater than the cost of providing psychotherapy? If so, we would be able to conclude that psychotherapy has a total cost offset.
Findings from meta-analyses and narrative reviews of the cost-offset literature provide explanations on these questions. In a meta-analysis of 91 studies conducted between 1967 and 1997, Chiles et al. (1999) found that psychotherapy and psychological interventions led to significant medical cost offsets. Participants in reviewed studies included surgery inpatients, high health-service users, and people with psychological and substance use disorders who received psychotherapy or psychological interventions alone or as part of a multimodal programme. Chiles and his team found that medical cost offsets occurred in 90% of studies and ranged from 20% to 30%. In 93% of studies where data were provided, cost offsets exceeded the cost of providing psychotherapy. Greater costs offsets occurred for older inpatient who required surgery, oncology, and cardiac rehabilitation than for outpatients who required care for minor injuries and illnesses. Structured psychological interventions, tailored to patient needs associated with their medical conditions, led to greater medical cost offsets than traditional psychotherapy.
In a set of meta-analyses from earlier studies involving Blue Cross and Blue Shield US Federal Employees Plan claim files and 58 controlled studies, Mumford et al. (1984) found that 85% of studies medical cost offset for psychotherapy occurred, and this was due to shorter periods of hospitalisation for surgery, cancer, heart disease and diabetes – particularly in patients over the age of 55. In a review of psychological interventions for people with a variety of health-related difficulties, Groth-Marnat and Edkins (1996) found that medical cost offsets occurred when such interventions targeted patients preparing for surgery and patients with difficulty adhering to medical regimens. Medical offset also occurred for smoking cessation programmes, rehabilitation programmes, and programmes for patients with chronic pain disorders, cardiovascular disorders and psychosomatic complaints.
Three other important reviews of medical cost-offset literature, which focussed largely on mental health problems in adults rather than adjustment to physical illness, deserve mention. In a review of 30 studies of psychotherapy for psychological disorders and drug and alcohol abuse, Jones and Vischi (1979) found that medical cost offsets occurred in most cases. In a review of eight cost-effective studies for substance abuse, Morgan and Crane (2010) concluded that family-based treatments can be cost-effective. In a review of 18 studies of psychotherapy for psychological disorders, Gabbard et al. (1997) found that in more than in 80% of studies, medical cost offsets exceeded the cost of providing psychological therapies. Significant cost-offsets occurred for complex problems and in studies of psychoeducational family therapy for schizophrenia and dialectical behaviour therapy for personality disorders this was achieved by reducing the need for inpatient care and improving occupational adjustment.

Besides the impact on people’s well-being, the report estimates the total costs of mental ill-health at over EUR 600 billion – or more than 4% of GDP – across Europe / Source: OECD Library

Prevalence by Mental and Substance use disorder / Source: OurWorldinData

The table provides a brief summary of the data which follows on mental health and substance use disorders / Source: OurWorldinData

Source: The Poverty Site
Therefore, to conclude with all the evidence reviewed here, it is widely accepted today that psychotherapeutic interventions have a significant medical cost offset. Those who participate in psychotherapy use fewer extra medical services at primary, secondary and tertiary levels and are hospitalised less than those who do not receive psychotherapy.
_____________________________________
*****
Bibliography
- American Psychiatric Association (2000). Diagnostic and Statistical Manual of the Mental Disorders (fourth edition, text revision, DSM-IV-TR). Washington. DC: APA.
- American Psychiatric Association (2006). American Psychiatric Association practice guidelines for the treatment of eating disorders (third revision). Washington, DC: APA.
- Angst, J. (2009). Course and prognosis of mood disorders. In M. Gelder et al. (Eds.), New Oxford textbook of psychiatry (second edition, Vol. 1, pp. 665-669). Oxford: Oxford University Press.
- Antony, M., & Stein, M. (2009a). Oxford Handbook of anxiety and related disorders. New York: Oxford University Press.
- Antony, M., & Stein, M. (2009b). Future directions in anxiety disorders research. In M. M. Antony & M. B. Stein (Eds.), Oxford handbook of anxiety and related disorders (pp. 667-677). New York: Oxford University Press.
- Ballenger, J. (2009). Panic disorder and agoraphobia. In M. Gelder et al. (Eds.), New Oxford textbook of psychiatry (second edition, Vol. 1, pp. 750-765). Oxford: Oxford University Press.
- Bech, P. (2009). Clinical features of mood disorders and mania. In M. Gelder et al. (Eds.), New Oxford textbook of psychiatry (second edition, Vol. 1, pp. 632-637). Oxford: Oxford University Press.
- Berman, A. (2009). Depression and suicide. In H. Gotlib & C. Hammen (Eds.), Handbook of depression (second edition, pp. 510-533). New York: Guilford Press.
- Bitran, S., Barlow, D., & Spiegel, D. (2009). Generalized anxiety disorders. In M. Gelder et al. (Eds.), New Oxford Textbook of Psychiatry (second edition, Vol. 1, pp. 729-739). Oxford University Press.
- Boland, R. J., & Keller, M. B. (2009). Course and outcome of depression. In H. Gotlib & C. Hammen (Eds.) Handbook of depression (second edition, pp. 23-43). New York: Guilford Press.
- Bota, R., Munro, S., Nguyen, C., & Preda, A. (2011). The course of schizophrenia : What has been learned from longitudinal studies ? In M. Ritsner (Ed.), Handbook of schizophrenia spectrum disorders, Volume II. Phenotypic and endophenotypic presentations (pp. 281-300). New York: Springer
- Brent, D., & Weersing, R. (2008). Depressive disorders in childhood and adolescents. In M. Rutter et al. (Eds.), Rutter’s child and adolescent psychiatry (fifth edition, pp. 587-612). London: Blackwell.
- Carr, A. (2012). Clinical psychology. 1st ed. New York: Routledge.
- Casey, R. J., & Berman, J. S., (1985). The outcome of psychotherapy with children. Psychological Bulletin, 98, 388-400.
- Caspi, O. (2004). How good are we? A meta-analytic study of effect sizes in medicine. Dissertation Abstracts International, Section B: The Sciences and Engineering, 65(5-B), 2607.
- Chiles, J., Lambert, M. & Hatch, A. (1999). The impact of psychological interventions on medical cost offset: A meta-analytic review. Clinical Psychology: Science and Practice, 6, 204-220.
- Cohen, J. (1988). Statistical power analysis for the behavioural sciences (second edition). Hillsdale, NJ: Lawrence Erlbaum Associates.
- DiMaggio, C., & Galea, S. (2006). The behavioural consequences of terrorism: A meta-analysis. Academy of Emergency Medicine, 13, 559-566.
- Ehlers, A. (2009). Post-traumatic stress disorder. In M. Gelder et al. (Eds.), New Oxford textbook of psychiatry (second edition, Vol. 1, pp 700-713). Oxford: Oxford University Press.
- Elliot, R., Greenberg, L. & Lietaer, G. (2004). Research on experiential psychotherapies. In M. Lambert (ed.), Bergin and Garfield’s handbook of psychotherapy and behaviour change (fifth edition, pp. 493-539). New York: Wiley.
- Friedman, M. J. (2009). Phenomenology of posttraumatic stress disorder and acute stress disorder. In M. M. Antony & M. B. Stein (Eds.), Oxford handbook of anxiety and related disorders (pp. 65-72). New York: Oxford University Press.
- Furr, J. M., Tiwari, S., Suveg, C., & Kendall, P. C. (2009). Anxiety Disorders in Children and Adolescents. In M. M. Antony & M. B. Sten (Eds.), Oxford handbook of anxiety and related disorders (pp 636-656). New York: Oxford University Press.
- Gabbard, G. O., Lazar, S.G., Hornberger, J. & Spiegel, D. (1997). The economic impact of psychotherapy: A review. American Journal of Psychiatry, 154, 147-155.
- Garber, J. (2010). Vulnerability to depression in childhood and adolescence. In R. Ingram and J. Price (Eds.), Vulnerability to psychopathology: Risk across the lifespan (second edition, pp. 189-247). New York: Guilford Press.
- Glass, V. (1976). Primary, secondary and meta-analysis of research. Educational Researcher, 5, 3-8.
- Golden, T., Gaynes, B., Ekstrom, D., Hamer, R., Jacobsen, F., Suppes, T., et al. (2005). The efficacy of light therapy in the treatment of mood disorders: A review and meta-analysis of the evidence. American Journal of Psychiatry, 162, 656-662.
- Gotlib, H., & Hammen, C. (2009). Handbook of depression (second edition). New York: Guilford Press.
- Grissom, R. (1996). The magical number. 7 +/- .2: Meta-meta-analysis of the probability of superior outcome in comparisons involving therapy, placebo and control. Journal of Consulting and Clinical Psychology, 64, 973-982.
- Groth-Marnat, G. & Edkins, G. (1996). Professional psychologists in general health care settings: A review of financial efficacy of direct treatment interventions. Professional Psychology: Research and Practice, 27, 161-174.
- Häfner, H., & an der Heiden, W. (2008). Course and outcome. In K. Mueser & D. Jeste (Eds.), Clinical handbook of schizophrenia (pp. 100-116). New York: Guilford Press.
- Halmi, K. A. (2010). Psychological comorbidity of eating disorders. In W. S. Agras (Ed.), The Oxford handbook of eating disorders (pp. 292-303). New York: Oxford University Press.
- Hammen, C., Bistricky, S., & Ingram, R. (2010). Vulnerability to depression in adulthood. In R. Ingram and J. Price (Eds.), Vulnerability to psychopathology: Risk across the lifespan (second edition, pp. 248-281). New York: Guilford Press.
- Hazlett-Stevens, H., Pruitt, L. D., & Collins, A. (2009). Phenomenology of generalized anxiety disorders. In M. M. Antony & M. B. Sten (Eds.), Oxford handbook of anxiety and related disorders (pp. 47 – 55). New York: Oxford University Press.
- Heisel, M. J. (2008). Suicide. In K. Mueser & D. Jeste (Eds.), Clinical handbook of schizophrenia (pp. 491-506). New York: Guilford Press.
- Hofmann, S. G., Alpers, G. W., & Pauli, P. (2009). Phenomenology of panic and phobic disorders. In M. M. Antony & M. B. Stein (Eds.), Oxford handbook of anxiety and related disorders (pp. 34 – 46). New York: Oxford University Press.
- Huppert, J. D. (2009). Anxiety disorders and depression comorbidity. In M. M. Antony & M. B. Stein (Eds.), Oxford handbook of anxiety and related disorders (pp. 576-586). New York: Oxford University Press.
- Jablensky, A. (2009). Course and outcome of schizophrenia and their prediction. In M. Gelder et al. (Eds.), New Oxford textbook of psychiatry (second edition, Vol. 1, pp 568 – 578). Oxford: Oxford University Press.
- Joiner, T., & Timmons, K. A. (2009). Depression in its interpersonal context. In H. Gotlib & C. hammen (Eds.) Handbook of depression (second edition, pp. 322-339). New York: Guilford Press.
- Jones, K. & Vischi, T. (1979). The impact of alcohol, drug abuse, and mental health treatment on medical care utilization: A review of the research literature. Medical Care, 17 (Suppl. 12), 43-131.
- Joormann, J. (2009). Cognitive aspects of depression. In H. Gotlib & C. Hammen (Eds.), Handbook of depression (second edition, pp. 298-321). New York: Guilford Press.
- Kazdin, A., Bass, D., Ayers, W., & Rodgers, A. (1990). Empirical and clinical focus of child and adolescent psychotherapy research. Journal of Consulting and Clinical Psychology, 58, 729-740.
- Kessler, R., & Wang, P. S. (2009). Epidemiology of depression. In H. Gotlib & C. Hammen (eds.), Handbook of depression (second edition, pp. 5 – 22). New York: Guilford Press.
- Kessler, R., Berglund, P., Demler, O., Jin, R., Merikangas, K. & Walters, E. (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62, 593-602.
- Kessler, R., Ruscio, A. M., Shear, K., & Wittchen, H. (2009). Epidemiology of anxiety disorders. In M. M. Antony & M. B. Sten (Eds.) Oxford handbook of anxiety and related disorders (pp. 19-33). New York: Oxford University Press.
- Lambert, M. & Ogles, B. (2004). The efficacy and effectiveness of psychotherapy. In M.J. Lambert (Ed.), Bergin and Garfield’s handbook of psychotherapy and behaviour change (fifth edition, pp. 139-193). New York: Wiley
- Leichsenring, F. & Rabung, S. (2011). Long-term psychodynamic psychotherapy in complex mental disorders: A meta-analysis. British Journal of Psychiatry, 199, 15-22.
- Leichsenring, F., Rabung, S. & Leibing, E. (2004). The efficacy of short-term psychodynamic psychotherapy in specific psychiatric disorders: A meta-analysis. Archives of General Psychiatry, 61, 1208-1216.
- Levison, D. F. (2009). Genetics of major depression. In H. Gotlib & C. Hammen (Eds.), Handbook of depression (second edition, pp 165-186). New York: Guilford Press.
- Lilienfeld, S. (2007). Psychological treatments that cause harm. Perspectives on Psychological Science, 2, 53-70.
- Liu, R. T., & Alloy, L. B. (2010). Stress generation in depression: A systematic review of empirical literature and recommendations for future study. Clinical Psychology Review, 30, 582-593.
- Luty, J., Fekadu, D., & Dhandayudham, A. (2006). Understanding of the term ‘schizophrenia’ by the British public. Psychiatric Bulletin, 30, 435-435.
- Mathews, C. A. (2009). Phenomenology of obsessive-compulsive disorder. In M. M. Antony & M. B. Stein (Eds.), Oxford handbook of anxiety and related disorders (pp. 56-64). New York: Oxford University Press.
- McGrath, J., Saha, S., Welham, J., Saadi, O., MacCauley, C., & Chant, D. (2004). A systematic review of the incidence of schizophrenia: The distribution of rates and the influence of sex, urbanicity, migrant status and methodology. BMC Medicine, 2, 13.
- Monroe, S., Slavich, G. M., & Georgiades, K. (2009). The social environment and life stress in depression. In H. Gotlib & C. Hammen (Eds.), Handbook of depression (second edition, pp. 340-360). New York: Guilford Press.
- Morgan, T. B. & Crane, D. R. (2010). Cost-effectiveness of family-based substance abuse treatment. Journal of Marital and Family Therapy, 36, 486-498.
- Mueser, K. & Duva, S. (2011). Schizophrenia. In D. Barlow (ed.), The Oxford handbook of clinical psychology (pp. 469-503). New York: Oxford University Press.
- Mueser, K., & Jeste, D. (2008). Clinical handbook of schizophrenia. New York: Guilford Press.
- Mumford, E., Schlesinger, H., Glass, G., Patrick, C. & Cuerton, T. (1984). A new look at evidence about reduced cost of medical utilization following mental health treatment. American Journal of Psychiatry, 141, 1145-1158.
- Murray, C., & Lopez, A. (1996). The global burden of disease, injuries and risk factors in 1990 and projected to 2020. Cambridge, MA: Harvard University Press.
- Murray, R., & Lewis, S. (1987). Is schizophrenia a neurodevelopmental disorder? British Medical Journal, 295, 681-682.
- Murray, R., & Van Os, J. (1998). Predictors of outcome in schizophrenia. Journal of Clinical Psychopharmacology, 18, 25-45.
- Noken-Hoeksema, S., & Hilt, L. M. (2009b). Handbook of depression in adolescents. New York: Guilford Press.
- Norcross, J., Beutler, L., & Levant, R. (2006). Evidence-based practices in mental health: Debate and dialogue on the fundamental questions. Washington, DC: American Psychological Association.
- Ozer, E., Best, S., Lipsey, T., & Weiss, D. (2003). Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psychological Bulletin, 129, 52-73
- Parker, G. (2009). Diagnosis, classification and differential diagnosis of the mood disorders. In M. Gelder et al (Eds.) New Oxford textbook of psychiatry (second edition, Vol. 1, pp. 637-645). Oxford: Oxford University Press.
- Pine, D. & Klein, R. (2008). Anxiety Disorders. In M. Rutter et al (Eds.), Rutter’s child and adolescent psychiatry (fifth edition, pp. 628-647). London: Blackwell
- Rosenthal, N. E. (2009). Issues for DSM-V: Seasonal affective disorder and seasonality. American Journal of Psychiatry, 166, 852-853.
- Rosenthal, R. & Rubin, D. (1982). A simple, general purpose display of magnitude of experimental effect. Journal of Educational Psychology, 74, 166-196.
- Sackett, D., Rosenberg, W., Gray, J., Haynes, R., & Richardson, W. (1996). Evidence-based medicine: What it is and what it isn’t. British Medical Journal, 312, 71-72.
- Sackett, D., Straus, S., Richardson, W., Rosenberg, W., & Haynes, R. (2000). Evidence based medicine: How to practice and teach EBM (second edition). London: Churchill Livingstone.
- Saha, S., Chant, D., Welham, J., & McGrath, J. (2005). A systematic review of the prevalence of schizophrenia. PLoS Medicine, 2, 413-433.
- Schennach-Wolff, R., Seemuller, F., Musil, R., Spellmann, I., Holler, H., & Riedel, M. (2011). Suicidality and the outcome of schizophrenia. In M. Ritsner (Ed.), Handbook of schizophrenia spectrum disorders, Volume III: Therapeutic approaches, comorbidity and outcome (pp. 365-382). New York: Springer.
- Shapiro, D. A., & Shapiro, D. (1982). Meta-analysis of comparative therapy outcome studies: A replication and refinement. Psychological Bulletin, 92, 581-604.
- Silvia, P.J., & Kaufman, J.C. (2010). Creativity and mental illness. In J. Kaufman & R. Sternberg (Eds.), The Cambridge handbook of creativity (pp. 381-394). New York: Cambridge University Press.
- Smith, M., & Glass, G. (1977). Meta-analysis of psychotherapy outcome studies. American Psychologist, 32, 752-760.
- Tandon, R., Nasrallah, H. A., & Keshavan, M. S. (2009). Schizophrenia, “just the facts” 4. Clinical features and conceptualisation. Schizophrenia Research, 110, 1-23.
- Vahia, I. V., & Cohen, C. I. (2008). Psychopathology. In K. Mueser & D. Jeste (Eds.), Clinical handbook of schizophrenia (pp. 82-90). New York; Guilford Press.
- Wampold, B. (2001). The great psychotherapy debate: Models, Methods, and findings. Mahwah, NJ: Lawrence Erlbaum Associates.
- Weisz, J., Weiss, B., Alicke, M., & Klotz, M. (1987). Effectiveness of psychotherapy with children and adolescents: A meta-analysis for clinicians. Journal of Consulting and Clinical Psychology, 55, 542-549.
- Weisz, J., Weiss, B., Han, S. & Granger, D. (1995). Effects of psychotherapy with children and adolescents revisited: A meta-analysis of treatment outcome studies. Psychological Bulletin, 117, 450-468.
- Wierzbicki, M. & Pekarik, G. (1993). A meta-analysis of psychotherapy dropout. Professional Psychology: Research & Practice, 24, 190-195.
- World Health Organization (1992). The ICD-10 Classification of Mental and Behavioural Disorders. Geneva, Switzerland: WHO.
- Zahradnik, M., & Stewart, S. H. (2009). Anxiety disorders and substance use disorder comorbidity. In M. M. Antony & M. B. Stein (Eds.), Oxford handbook of anxiety and related disorders (pp. 565-575). New York: Oxford University Press.
- Zohar, J., Fostick, L. & Juven-Wetzler, E. (2009). Obsessive-compulsive disorder. In M. Gelder et al. (Eds.), New Oxford textbook of psychiatry (second edition, Vol. 1, pp. 765-774). Oxford: Oxford University Press.
- Zubin, J., & Spring, B. (1977). Vulnerability: A new view of schizophrenia. Journal of Abnormal Psychology, 86, 103-126.
Danny J. D’Purb | DPURB.com
____________________________________________________
While the aim of the community at dpurb.com has been & will always be to focus on a modern & progressive culture, human progress, scientific research, philosophical advancement & a future in harmony with our natural environment; the tireless efforts in researching & providing our valued audience the latest & finest information in various fields unfortunately takes its toll on our very human admins, who along with the time sacrificed & the pleasure of contributing in advancing our world through sensitive discussions & progressive ideas, have to deal with the stresses that test even the toughest of minds. Your valued support would ensure our work remains at its standards and remind our admins that their efforts are appreciated while also allowing you to take pride in our journey towards an enlightened human civilization. Your support would benefit a cause that focuses on mankind, current & future generations.
Thank you once again for your time.
Please feel free to support us by considering a donation.
Sincerely,
The Team @ dpurb.com
P.S.
– If you are a group/organization or individual looking for consultancy services, email: info[AT]dpurb.com
– If you need to reach Danny J. D’Purb directly for any other queries or questions, email: danny[AT]dpurb.com [Inbox checked periodically / Responses may take up to 20 days or more depending on his schedule]
Stay connected by linking up with us on Facebook and Twitter





Psychoanalysis: History, Foundations, Legacy, Impact & Evolution
In contemporary psychology, the psychoanalytic movement’s place is both unique and paradoxical. Focussing on the study of the mind as a “software” running on the brain as the “hardware”, psychoanalysis remains the only discipline that truly focuses on the mechanism and processes behind our thoughts. Unlike empirical behavioural science and other “cogno-sciences” that can be fairly barbaric and obstinate in the forced application of the rigid mathematical and systematic procedures embedded in the classic scientific method when dealing with an entity as complex and organic as the human mind; psychoanalysis has remained focussed in understanding human psychology by capturing it in all its details, depths, dimensions and linguistic aspects.
The scientific method although a proven mathematical approach to inquiries in the hard sciences [e.g. biology, medecine, physics, chemistry, astrophysics, material science, astronomy, etc], shows its limitations when used as a tool for psychological inquiry in the measurement of variables that are incredibly hard to measure such as emotions, values, motives, desires, libidinous intensity or dreams. It is also fair noting that humans are different from simple organisms, molecules or robots, hence psychoanalysis remains the only discipline focused on the mind [the software] assuming that most human beings have a physiologically healthy brain [the hardware]…
Read in full here: https://dpurb.com/2018/11/18/essay-psychoanalysis-history-foundations-legacy-impact-evolution/
_____________________________________________________
_____________________________________________________
Developmental Psychology: The 3 Major Theories of Childhood Development
In 1984, Nicholas Humphrey described us as “nature’s psychologists’” or homo psychologicus. What he meant was that as intelligent social beings, we tend to use our knowledge of our own thoughts and feelings – “introspection” – as a guide for understanding how others are likely to think, feel and hence, behave. He also argued that we are conscious [i.e. we have self-awareness] precisely because such an attribute is useful in the process of understanding others and having a successful social existence – consciousness is a biological adaptation that enables us to perform introspective psychology. Today, we are confident in the knowledge that the process of understanding others’ thoughts, feelings and behaviour is an ability that develops through childhood and most likely throughout our lives; and according to the greatest child psychologist of all time, Jean Piaget, a crucial phase of this process occurs in middle childhood.
Developmental psychology can be characterised as the field that attempts to understand and explain the changes that happen over time in the thought, behaviour, reasoning and functioning of a person due to biological, individual and environmental influences. Developmental psychologists study children’s development, and the development of human behaviour across the organism’s lifetime from a variety of different perspectives. Hence, if we are studying different areas of development, different theoretical perspectives will be fundamental and may influence the ways psychologists and scholars think about and study development.
Through the systematic collection of knowledge and experiments, we can develop a greater understanding and awareness of ourselves than would otherwise be possible…
Full Article: https://dpurb.com/2018/07/15/developmental-psychology-the-3-major-theories-of-development/
_____________________________________________________
https://twitter.com/NietzscheAcadem/status/856610013825167360
_____________________________________________________
Listening to classical music modulates genes that are responsible for brain functions
A Finnish study group has investigated how listening to classical music affected the gene expression profiles of both musically experienced and inexperienced participants. All the participants listened to W.A. Mozart’s violin concert Nr 3, G-major, K.216 that lasts 20 minutes.
Listening to music enhanced the activity of genes involved in dopamine secretion and transport, synaptic function, learning and memory. One of the most up-regulated genes, synuclein-alpha (SNCA) is a known risk gene for Parkinson’s disease that is located in the strongest linkage region of musical aptitude. SNCA is also known to contribute to song learning in songbirds.
“The up-regulation of several genes that are known to be responsible for song learning and singing in songbirds suggest a shared evolutionary background of sound perception between vocalizing birds and humans”, says Dr. Irma Järvelä, the leader of the study.
In contrast, listening to music down-regulated genes that are associated with neurodegeneration, referring to a neuroprotective role of music.
“The effect was only detectable in musically experienced participants, suggesting the importance of familiarity and experience in mediating music-induced effects”, researchers remark.
The findings give new information about the molecular genetic background of music perception and evolution, and may give further insights about the molecular mechanisms underlying music therapy.
Kanduri, C., Raijas, P., Ahvenainen, M., Philips, A., Ukkola-Vuoti, L., Lähdesmäki, H. and Järvelä, I. (2015). The effect of listening to music on human transcriptome. PeerJ, 3, p.e830.
__________________________________
_____________________________________________________
Why Kids With High IQs Are More Likely to Take Drugs
People with high IQs are more likely to smoke marijuana and take other illegal drugs, compared with those who score lower on intelligence tests, according to a new study from the U.K.
“It’s counterintuitive,” says lead author James White of the Center for the Development and Evaluation of Complex Interventions for Public Health Improvement at Cardiff University in Wales. “It’s not what we thought we would find.”
The IQ effect was larger in women: women in the top third of the IQ range at age 5 were more than twice as likely to have taken marijuana or cocaine by age 30, compared with those scoring in the bottom third. The men with the highest IQs were nearly 50% more likely to have taken amphetamines and 65% more likely to have taken ecstasy, compared to those with lower scores.
And these results held even when researchers controlled for factors like socioeconomic status and psychological distress, which are also correlated with rates of drug use.
So why might smarter kids be more likely to try drugs? “People with high IQs are more likely to score high on personality scales of openness to experience,” says White. “They may be more willing to experiment and seek out novel experiences.”
That could potentially be linked to the boredom and social isolation experienced by many gifted children, the authors note. But since a link between IQ and drug use remains independent of psychological distress, that can’t be all that’s going on. “It rules out the argument that the only reason people take illegal drugs is to self medicate,” says White…
White, J. and Batty, G. (2011). Intelligence across childhood in relation to illegal drug use in adulthood: 1970 British Cohort Study. Journal of Epidemiology & Community Health, 66(9), pp.767-774.
_____________________________________________________
Selective forgetting of unreliable information can have the positive side effect of reducing mental clutter
Forgetting is often considered to be bad, but selective forgetting of unreliable information can have the positive side effect of reducing mental clutter, thereby making it easier to access our most important memories. Prior studies of forgetting have focused on passive mechanisms (decay, interference) or on effortful inhibition by cognitive control. Here we report the discovery of an active mechanism for forgetting that weakens memories selectively and without burdening the conscious mind. Specifically, we show that the brain automatically generates predictions about which items should appear in familiar contexts; if these items fail to appear, their memories are weakened. This process is adaptive, because such memories may have been encoded incorrectly or may represent unstable aspects of the world.
Kim, G., Lewis-Peacock, J., Norman, K. and Turk-Browne, N. (2013). Pruning of visual memories based on contextual prediction error. Journal of Vision, 13(9), pp.930-930.
_____________________________________________________
Could there be a bright side to depression?
The researchers administered their test to nearly 600 subjects. Their paper, “Measuring the bright side of being blue”, appears in the peer-reviewed, open access journal PLOS ONE.
The researchers at McMaster and the Centre for Addiction and Mental Health were able to show a meaningful connection between answers to a 20-question test and analytical rumination – a type of distraction-resistant thinking that is characteristic of clinical and sub-clinical depression alike…
Barbic, S., Durisko, Z. and Andrews, P. (2014). Measuring the Bright Side of Being Blue: A New Tool for Assessing Analytical Rumination in Depression. PLoS ONE, 9(11), p.e112077.
_____________________________________________________
_____________________________________________________
Being depressed can be deadly for young women who have a heart attack
http://www.futurity.org/depression-heart-disease-death-women-719342/
_____________________________________________________
Effect of Music Therapy on the Anxiety Levels and Sleep Patterns of Abused Women in Shelters
Extract:
The purpose of this study was to explore the effect of a music therapy procedure (music listening paired with progressive muscle relaxation) on the reduction of anxiety and improvement of sleep patterns in abused women in shelters. Twenty-eight women residing in 2 domestic violence shelters in a Midwestern city met with the researcher on 5 consecutive days for half-hour sessions. A pretest-posttest design with control and experimental groups was used. The dependent variables included: stait anxiety measured by the STAI (Spielberger et al., 1983) before and after each music stimulus, sleep quality as measured by the PSQI (Buysse et al., 1989) on the first and last sessions, and levels of fatigue as measured by the Fatigue Scale (Lee, 1992) at waking time. The independent variable was a 20-minute recording of participant-selected music with a Progressive Muscle Relaxation script. Results indicated that music therapy constituted an effective method for reducing anxiety levels. Results also indicated a significant effect on sleep quality for the experimental group, but not for the control group. No significant relationships were found between anxiety levels and sleep quality, nor fatigue levels and sleep quality. These results seem promising in the light of domestic violence research, which has found that a greater amount of personal resources is a crucial aspect of abused women’s recovery process. Reduction of anxiety and improvement of sleep quality can be considered as increased personal resources, and seem feasible through the use of music therapy.
Hernandez-Ruiz, E. (2005). Effect of Music Therapy on the Anxiety Levels and Sleep Patterns of Abused Women in Shelters. Journal of Music Therapy, 42(2), pp.140-158.
_____________________________________________________
https://twitter.com/Volpones1/status/920619244546609152
_____________________________________________________
https://twitter.com/AHistoryofArt/status/929782360555577346
__________________________________
Nos intelligences multiples : comment mieux intégrer les personnes autistes?
Et si l’autisme était une preuve d’intelligence à part ? Comment faire pour que cette forme d’intelligence soit respectée ? En philosophe, Josef Schovanec a accepté de nous livrer sa propre expérience de l’autisme.
Depuis les années 80, la psychologie a montré que l’intelligence n’était pas une donnée mesurable. Les autistes ont beaucoup souffert de ces tests mis en place par la société. Et si l’autisme était une preuve d’intelligence à part ? Comment faire pour que cette forme d’intelligence soit respectée ? En philosophe, Joseph Schovanec a accepté de nous livrer sa propre expérience de l’autisme.
Article: https://www.franceculture.fr/emissions/les-chemins-de-la-philosophie/nos-intelligences-multiples-comment-mieux-integrer-les-personnes-autistes
__________________________________
__________________________________
Warm thanks: Gratitude expression facilitates social affiliation in new relationships via perceived warmth.
Abstract:
Recent theorizing on the nature and function of gratitude (the find-remind-and-bind theory; Algoe, 2012) stipulates that expressing gratitude should serve to alert previously unacquainted peers to the potential for a high-quality social bond (i.e., a find function). Although the logic of this premise is supported by extant research, it has not, as yet, been tested empirically. In the current study, participants received a note from a previously unacquainted peer that contained an expression of gratitude (or did not) with regard to prior benefits provided by the participant. After providing ratings of the peer and ostensibly completing the study, participants were given an opportunity to spontaneously give their contact information to the peer, which served as a behavioral measure of affiliation. In line with the proposed find function of gratitude expressions, recipients of expressions of gratitude were more likely to extend the effort to continue the relationship with the novel peer by providing that peer with a means to contact them. This experiment also provided evidence that perceptions of interpersonal warmth (e.g., friendliness, thoughtfulness) serve as the mechanism via which gratitude expressions facilitate affiliation: insofar as gratitude expressions signaled interpersonal warmth of the expresser, they prompted investment in the burgeoning social bond. As such, these findings provide the first empirical evidence regarding 1 of the 3 central premises of the find-remind-and-bind theory of gratitude (Algoe, 2012) in the context of novel relationships.
Williams, L. and Bartlett, M. (2015). Warm thanks: Gratitude expression facilitates social affiliation in new relationships via perceived warmth. Emotion, 15(1), pp.1-5.
__________________________________
Functional Neural Plasticity and Associated Changes in Positive Affect After Compassion Training
Abstract:
The development of social emotions such as compassion is crucial for successful social interactions as well as for the maintenance of mental and physical health, especially when confronted with distressing life events. Yet, the neural mechanisms supporting the training of these emotions are poorly understood. To study affective plasticity in healthy adults, we measured functional neural and subjective responses to witnessing the distress of others in a newly developed task (Socio-affective Video Task). Participants’ initial empathic responses to the task were accompanied by negative affect and activations in the anterior insula and anterior medial cingulate cortex—a core neural network underlying empathy for pain. Whereas participants reacted with negative affect before training, compassion training increased positive affective experiences, even in response to witnessing others in distress. On the neural level, we observed that, compared with a memory control group, compassion training elicited activity in a neural network including the medial orbitofrontal cortex, putamen, pallidum, and ventral tegmental area—brain regions previously associated with positive affect and affiliation. Taken together, these findings suggest that the deliberate cultivation of compassion offers a new coping strategy that fosters positive affect even when confronted with the distress of others.
Klimecki, O., Leiberg, S., Lamm, C. and Singer, T. (2012). Functional Neural Plasticity and Associated Changes in Positive Affect After Compassion Training. Cerebral Cortex, 23(7), pp.1552-1561.
__________________________________
Affective Priming
Extract:
“This blog presents a third example of priming known generally as the affective priming, also known as emotional priming. On page 230 of my book, Cognitive Neuroscience and Psychotherapy: Network Principles for a Unified Theory, I describe emotional priming as follows:
Emotional priming entails the repeated presentation of words that activate emotions. For example, Power et al. (1991) used sets of words to activate the following four basic emotions: (a) happiness, love, joy, pleasure; (b) sadness, grief, misery, depression; (c) anger, hate, jealousy, aggression; and (d) fear, panic, terror, anxiety…
Affective priming is a robust method for activating brain mechanisms that modify how we think and feel about a wide variety of matters…
Full Article: http://scitechconnect.elsevier.com/affective-priming/
“Progress is impossible without change, & those who cannot change their minds cannot change anything.” -GB Shaw
Don’t let your mind be occupied by blame towards others. A liberated mind is a forgiving one.
“Change Your Attachment Style to Have a Better Life” by Dr. L. Firestone
“What if we could identify the filter that shapes our perception of the world and change it so as to have a better life? We are born into the social context of our families and quickly need to /develop strategies to get our needs met by our caretakers. Depending on our early emotional environment, we make the best adaptation to get our needs met by the potential caretakers we have available to us, usually our parents or other relatives. We are incredibly adaptive creatures, which is quite possibly our most unique feature as humans. Our early interactions create internal working models of how our future relationships will transpire and of how we will go about getting our needs met. Research has demonstrated that these childhood relationships shape our perceptions of others and our understanding of their minds and motives. These internal working models also influence the ways others are likely to treat us and perceive us…”
Full Article: https://www.psychalive.org/change-attachment-style-better-life/
“Savoir Aimer” courtesy of Florent Pagny // Album: Savoir Aimer (1997)
“It is the artist who tries to gradually accustom people to the possibilities of a better state of things.” ― C.A. Dawson Scott
_______________________________________________
_______________________________________________
Norms, self-sanctioning, and contributions to the public good
Abstract:
The relationship between norms, self-sanctioning, and people’s decisions about contributing to public goods is complex and often misunderstood in the public goods literature. We develop a model in which individuals self-sanction (e.g. feel guilty) for contributing less than a subjective norm level of contribution to a public good. From the model we derive the following testable hypotheses: an increase in one’s perception of the norm level of contribution to the public good (1) induces negative self-sanctioning and (2) will lead one to contribute more to the public good, and (3) that contributing to the public good induces positive self-sanctioning. To test these hypotheses, we elicit stated preferences for contributions to an organization which offsets carbon emissions and a proxy for self-sanctioning, respondent “self-image.” We fail to reject each hypothesis. Our results complement existing studies on how to encourage contributions to the public good.
Interis, M. and Haab, T. (2014). Norms, self-sanctioning, and contributions to the public good. Journal of Environmental Psychology, 38, pp.271-278.
_____________________________________________________
“Il est impossible de concevoir un système si parfait que personne ne doit être bon.”- T.S. Eliot
Traduction(EN):“It is impossible to design a system so perfect that no-one needs to be good.”
— T.S. Eliot
_____________________________________________________
_____________________________________________________
_____________________________________________________
_____________________________________________________
Gary Bourlet explains why Learning Disability England supports the Learning Disability and Autism Leaders’ Award 2019.
_____________________________________________________
In A Month
https://twitter.com/Statista_UK/status/888336521505513472
____________________________________________
Depression increases heart failure risk by 40 percent
Moderate to severe depression increases the risk of heart failure by 40 percent, a study of nearly 63,000 Norwegians has shown. During the study period nearly 1,500 people developed heart failure. Compared to residents with no symptoms of depression, people with mild symptoms had a 5% increased risk of developing heart failure and those with moderate to severe symptoms had a 40% increased risk.
Article: https://www.sciencedaily.com/releases/2014/04/140404140203.htm
____________________________________________
___________________________________________________
How do you define #wellbeing? See what others have to say
#ModernSociety #World #Edu
http://www.oecdbetterlifeindex.org/#/11111111111
Adoption of new #technology since 1900 in th #US
#Society #Consumer #Culture
http://bit.ly/19wkABd
_____________________________________________________
#Success as #LOW as 30% when promoting #finance #people to broader #leadership roles
http://sloanreview.mit.edu/article/leading-by-the-numbers//
_____________________________________________________
Religiosity and Major Depression in Adults at High Risk: A Ten-Year Prospective Study
Abstract:
Objective
Previously the authors found that personal importance of religion or spirituality was associated with a lower risk for major depression in a study of adults with and without a history of depression. Here the authors examine the association of personal importance of religion or spirituality with major depression in the adult offspring of the original sample using a 10-year prospective longitudinal design.
Method
Participants were 114 adult offspring of depressed and nondepressed parents, followed longitudinally. The analysis covers the period from the 10-year to the 20-year follow-up assessments. Diagnosis was assessed with the Schedule for Affective Disorders and Schizophrenia–Lifetime Version. Religiosity measures included personal importance of religion or spirituality, frequency of attendance at religious services, and denomination (all participants were Catholic or Protestant). In a logistic regression analysis, major depression at 20 years was used as the outcome measure and the three religiosity variables at 10 years as predictors.
Results
Offspring who reported at year 10 that religion or spirituality was highly important to them had about one-fourth the risk of experiencing major depression between years 10 and 20 compared with other participants. Religious attendance and denomination did not significantly predict this outcome. The effect was most pronounced among offspring at high risk for depression by virtue of having a depressed parent; in this group, those who reported a high importance of religion or spirituality had about one-tenth the risk of experiencing major depression between years 10 and 20 compared with those who did not. The protective effect was found primarily against recurrence rather than onset of depression.
Conclusions
A high self-report rating of the importance of religion or spirituality may have a protective effect against recurrence of depression, particularly in adults with a history of parental depression.
Miller, L., Wickramaratne, P., Gameroff, M., Sage, M., Tenke, C. and Weissman, M. (2012). Religiosity and Major Depression in Adults at High Risk: A Ten-Year Prospective Study. American Journal of Psychiatry, 169(1), pp.89-94.
_____________________________________________________
A diffusion tensor imaging study of brain microstructural changes related to religion and spirituality in families at high risk for depression
Abstract:
Introduction
Previously in a three‐generation study of families at high risk for depression, we found that belief in the importance of religion/spirituality (R/S) was associated with thicker cortex in bilateral parietal and occipital regions. In the same sample using functional magnetic resonance imaging and electroencephalograph (EEG), we found that offspring at high familial risk had thinner cortices, increased default mode network connectivity, and reduced EEG power. These group differences were significantly diminished in offspring at high risk who reported high importance of R/S beliefs, suggesting a protective effect.
Methods
This study extends previous work examining brain microstructural differences associated with risk for major depressive disorder (MDD) and tests whether these are normalized in at‐risk offspring who report high importance of R/S beliefs. Diffusion tensor imaging (DTI) data were selected from 99 2nd and 3rd generation offspring of 1st generation depressed (high‐risk, HR) or nondepressed (low‐risk, LR) parents. Whole‐brain and region‐of‐interest analyses were performed, using ellipsoidal area ratio (EAR, an alternative diffusion anisotropy index comparable to fractional anisotropy). We examined microstructural differences associated with familial risk for depression within the groups of high and low importance of R/S beliefs (HI, LI).
Results
In the LI group, HR individuals showed significantly decreased EAR in white matter regions neighboring the precuneus, superior parietal lobe, superior and middle frontal gyrus, and bilateral insula, supplementary motor area, and postcentral gyrus. In the HI group, HR individuals showed reduced EAR in white matter surrounding the left superior, and middle frontal gyrus, left superior parietal lobule, and right supplementary motor area. Microstructural differences associated with familial risk for depression in precuneus, frontal lobe, and temporal lobe were nonsignificant or less significant in the HI group.
Conclusion
R/S beliefs may affect microstructure in brain regions associated with R/S, potentially conferring resilience to depression among HR individuals.
Li, X., Weissman, M., Talati, A., Svob, C., Wickramaratne, P., Posner, J. and Xu, D. (2019). A diffusion tensor imaging study of brain microstructural changes related to religion and spirituality in families at high risk for depression. Brain and Behavior, Brain and Behaviour, 9(2), p.e01209.
_____________________________________________________
Neuroanatomical Correlates of Religiosity and Spirituality: A Study in Adults at High and Low Familial Risk for Depression
Abstract:
Importance: We previously reported a 90% decreased risk in major depression, assessed prospectively, in adult offspring of depressed probands who reported that religion or spirituality was highly important to them. Frequency of church attendance was not significantly related to depression risk. Our previous brain imaging findings in adult offspring in these high-risk families also revealed large expanses of cortical thinning across the lateral surface of the right cerebral hemisphere.
Objective: To determine whether high-risk adults who reported high importance of religion or spirituality had thicker cortices than those who reported moderate or low importance of religion or spirituality and whether this effect varied by family risk status.
Design, Setting, and Participants: Longitudinal, retrospective cohort, familial study of 103 adults (aged 18-54 years) who were the second- or third-generation offspring of depressed (high familial risk) or nondepressed (low familiar risk) probands (first generation). Religious or spiritual importance and church attendance were assessed at 2 time points during 5 years, and cortical thickness was measured on anatomical images of the brain acquired with magnetic resonance imaging at the second time point.
Main Outcomes and Measures: Cortical thickness in the parietal regions by risk status.
Results: Importance of religion or spirituality, but not frequency of attendance, was associated with thicker cortices in the left and right parietal and occipital regions, the mesial frontal lobe of the right hemisphere, and the cuneus and precuneus in the left hemisphere, independent of familial risk. In addition, the effects of importance on cortical thickness were significantly stronger in the high-risk than in the low-risk group, particularly along the mesial wall of the left hemisphere, in the same region where we previously reported a significant thinner cortex associated with a familial risk of developing depressive illness. We note that these findings are correlational and therefore do not prove a causal association between importance and cortical thickness.
Conclusions and Relevance: A thicker cortex associated with a high importance of religion or spirituality may confer resilience to the development of depressive illness in individuals at high familial risk for major depression, possibly by expanding a cortical reserve that counters to some extent the vulnerability that cortical thinning poses for developing familial depressive illness.
We previously reported a 90% decreased risk, assessed prospectively for 10 years, of developing major depressive disorder (MDD) in adult offspring of depressed probands (high familial risk [HR]) who said that religion or spirituality was highly important to them.1 Attendance at religious services and religious denomination did not decrease the risk of MDD. Among the same participants in our 25-year, longitudinal, multigenerational study of MDD who underwent magnetic resonance imaging (MRI), we identified large expanses of cortical thinning across the lateral surface of the right cerebral hemisphere and mesial wall of the left hemisphere in adult offspring of the HR group.2 These findings led us to explore whether the regions where cortical thinning was located in the HR adults would be thicker in those who report a high personal importance of religion or spirituality and whether these findings would be significantly more prominent in persons at HR compared with low familial risk (LR) for MDD. A relatively thicker cortex in these regions could potentially account for the protection against depression that religion or spirituality seem to afford. (For ease of reading, we will refer to the personal importance of religion or spirituality simply as importance.)
Numerous studies have found an inverse association between religiosity and depression, and additional studies have attempted to identify a neurobiological basis for religious and spiritual experiences.3-9 In healthy individuals, for example, transcranial magnetic stimulation of the temporoparietal regions evoked feelings of sensed presence.10 A study11 on older adults using structural MRI prospectively associated born-again status, life-changing religious experiences, and Catholicism with subsequent greater atrophy in the hippocampus. Several functional neuroimaging studies2,12-15 of healthy adults using functional MRI and single-photon emission computed tomography revealed that the intensity of self-evoked religious experiences during MRI was associated with increased blood flow in various subregions of the prefrontal and parietal cortices. These neurobiological correlates of religious and spiritual experiences, however, have yet to be investigated in terms of the risk and protective benefits that they confer for MDD.
In the present study, we followed adults for more than 30 years adults were at either HR or LR for MDD, during which time the participants self-reported importance and frequency of attendance at services and were assessed for symptoms of depression. We assessed the associations of importance with measures of cortical thickness measured on MRIs of the brain acquired at the 25-year follow-up. In addition to reporting thinner cortices in HR adults that averaged nearly 30% across the lateral surface of the right hemisphere and mesial wall of the left, we also previously reported that thinner cortices in the HR group were state independent (ie, a thinner cortex was independent of whether participants were ever depressed and therefore was likely an endophenotype for MDD) and that the cortical thickness mediated the associations of familial risk for MDD with inattention and difficulty recalling social stimuli, cognitive disturbances that in turn were associated with increased symptoms of anxiety and depression.2,15
We therefore hypothesized that adults with self-reported high importance compared with those with low or moderate importance would have thicker cortices in brain regions, which was previously identified as an endophenotype for familial MDD. Because we have previously found that the effects of religious importance in protecting against MDD are greater in HR compared with LR adults, we further hypothesized that the HR compared with the LR participants would have larger expanses of the brain in which cortical thickness correlated positively with religious importance.
Miller, L., Bansal, R., Wickramaratne, P., Hao, X., Tenke, C., Weissman, M. and Peterson, B. (2014). Neuroanatomical Correlates of Religiosity and Spirituality. JAMA Psychiatry, 71(2), p.128.
_____________________________________________________
Mindfulness practice leads to increases in regional brain gray matter density
Therapeutic interventions that incorporate training in mindfulness meditation have become increasingly popular, but to date, little is known about neural mechanisms associated with these interventions. Mindfulness-Based Stress Reduction (MBSR), one of the most widely used mindfulness training programs, has been reported to produce positive effects on psychological well-being and to ameliorate symptoms of a number of disorders.
Here, we report a controlled longitudinal study to investigate pre-post changes in brain gray matter concentration attributable to participation in an MBSR program. Anatomical MRI images from sixteen healthy, meditation-naïve participants were obtained before and after they underwent the eight-week program.
Changes in gray matter concentration were investigated using voxel-based morphometry, and compared to a wait-list control group of 17 individuals. Analyses in a priori regions of interest confirmed increases in gray matter concentration within the left hippocampus. Whole brain analyses identified increases in the posterior cingulate cortex, the temporo-parietal junction, and the cerebellum in the MBSR group compared to the controls. The results suggest that participation in MBSR is associated with changes in gray matter concentration in brain regions involved in learning and memory processes, emotion regulation, self-referential processing, and perspective taking.
Hölzel, B., Carmody, J., Vangel, M., Congleton, C., Yerramsetti, S., Gard, T. and Lazar, S. (2011). Mindfulness practice leads to increases in regional brain gray matter density. Psychiatry Research: Neuroimaging, 191(1), pp.36-43.
_____________________________________________________
Temporal Dynamics of the Default Mode Network Characterize Meditation-Induced Alterations in Consciousness
Extract:
« In this study, we analyzed the DMN microstate to understand the mechanisms of meditation-induced alterations in consciousness. By contrasting healthy controls (HCs) at rest against expert meditators at rest and during meditation, we explored both state and trait changes in DMN-microstate dynamics produced by meditation with a hypothesis that these could cause differential alterations in its duration and frequency. The state changes felt during meditation are usually described as a deep sense of calm peacefulness, cessation or slowing of mind’s internal dialog and conscious awareness merging completely with the object of meditation (Brown, 1977; Wallace, 1999). Alongside, long-term expertise in meditation also produces durable changes in neural dynamics, with improvements in mental and physical health presumably due to its trait effects (Chiesa and Serretti, 2010, 2011; Hofmann et al., 2010). Here, we describe changes in the spatial configuration of the DMN as a function of meditation, and show that state and trait influences on the temporal dynamics of the DMN microstate can indeed be dissociated…
…this reflected a trait effect of meditation, highlighting its role in producing durable changes in temporal dynamics of the DMN. Taken together, these findings shed new light on short and long-term consequences of meditation practice on this key brain network.
Panda, R., Bharath, R., Upadhyay, N., Mangalore, S., Chennu, S. and Rao, S. (2016). Temporal Dynamics of the Default Mode Network Characterize Meditation-Induced Alterations in Consciousness. Frontiers in Human Neuroscience, 10.
_____________________________________________________
Meditators have brains that are physically 7 yrs younger, on average, than non-meditators
http://digest.bps.org.uk/2016/04/experienced-meditators-have-brains-that.html
_____________________________________________________
https://twitter.com/DannyDPurb/status/864335047976828928
_____________________________________________________
_____________________________________________________
Can #Business leaders #benefit from studying great #writers?
http://goo.gl/dqWiLP
_____________________________________________________
https://twitter.com/DannyDPurb/status/817140824316186624
__________________________________
Scientists discover 1,000 new “intelligence genes”
Intelligence is associated with important economic and health-related life outcomes1. Despite intelligence having substantial heritability2 (0.54) and a confirmed polygenic nature, initial genetic studies were mostly underpowered3,4,5. Here we report a meta-analysis for intelligence of 78,308 individuals. We identify 336 associated SNPs (METAL P < 5 × 10−8) in 18 genomic loci, of which 15 are new. Around half of the SNPs are located inside a gene, implicating 22 genes, of which 11 are new findings. Gene-based analyses identified an additional 30 genes (MAGMA P < 2.73 × 10−6), of which all but one had not been implicated previously. We show that the identified genes are predominantly expressed in brain tissue, and pathway analysis indicates the involvement of genes regulating cell development (MAGMA competitive P = 3.5 × 10−6). Despite the well-known difference in twin-based heritability2 for intelligence in childhood (0.45) and adulthood (0.80), we show substantial genetic correlation (rg = 0.89, LD score regression P = 5.4 × 10−29). These findings provide new insight into the genetic architecture of intelligence.
Sniekers, S., Stringer, S., Watanabe, K., Jansen, P., Coleman, J., Krapohl, E., Taskesen, E., Hammerschlag, A., Okbay, A., Zabaneh, D., Amin, N., Breen, G., Cesarini, D., Chabris, C., Iacono, W., Ikram, M., Johannesson, M., Koellinger, P., Lee, J., Magnusson, P., McGue, M., Miller, M., Ollier, W., Payton, A., Pendleton, N., Plomin, R., Rietveld, C., Tiemeier, H., van Duijn, C. and Posthuma, D. (2017). Genome-wide association meta-analysis of 78,308 individuals identifies new loci and genes influencing human intelligence. Nature Genetics, 49(7), pp.1107-1112.
__________________________________
https://twitter.com/DarwinMonkey/status/1018514424095789064
https://twitter.com/NietzscheAcadem/status/1059489396305604613
___________________________________________
Profession psychanalyste
Extrait:
Et si on abandonnait notre obsession pour la mort pour miser sur la pulsion de vie ?
« La psychanalyse n’est rien d’autre qu’une mise à nu, opération que l’homme encore malade évite parce qu’elle lui arrache son masque, mais que l’homme guéri accueille comme une libération. » – Lettre ouverte à Freud (1931)
Lou Andreas-Salomé (1861-1937) était romancière, essayiste et psychanalyste. De sa pratique de la psychanalyse et de sa connaissance de Freud, que reste-t-il aujourd’hui ? De leur rencontre en 1912 à ses écrits sur le narcissisme en passant par ses réflexions sur la névrose, sait-on qu’en elle, l’inventeur de l’inconscient a vu une disciple, une amie, et même une alliée ?
C’était pourtant une alliée paradoxale, une disciple hérétique, qui avait perçu dans la psychanalyse la révolution de son époque, l’a pratiqué jusqu’à sa mort, mais y avait apporté une contradiction majeure et d’actualité : et si on avait accordé trop d’importance à la pulsion de mort, et pas assez à la pulsion de vie ?
Article sur France Culture: https://www.franceculture.fr/emissions/avoir-raison-avec-lou-andreas-salome/profession-psychanalyste
___________________________________________
___________________________________________
Open communication and emotional closeness linked to fewer low sexual interest problems
Extract:
British women living with a partner are more than twice as likely to lack interest in sex compared to men living with a partner, according to a new study published in the BMJ Open.
The nationally representative survey interviewed 6,669 women and 4,839 men aged between 16 and 74 who reported at least one sexual partner in the past year. Overall, 34 per cent of women and 15 per cent of men reported lacking interest in sex. Half of these people – 62 per cent of women and 53 per cent of men – said that they were distressed by their lack of interest in sex.
Those who found it always easy to talk about sex with their partner were less likely to report lacking interest. This was true for men as well as women.
Professor Cynthia Graham, of the Centre for Sexual Health Research at the University of Southampton and lead author on the paper, said: “Our findings show us the importance of the relational context in understanding low sexual interest in both men and women. For women in particular, the quality and length of relationship and communication with their partners are important in their experience of sexual interest. It highlights the need to assess and – if necessary – treat sexual interest problems in a holistic and relationship-, as well as gender-specific way.”
The study also revealed other things linked to low interest in sex in men and women:
– Reporting an STI in the last year
– Ever experiencing sex against your will
– Poor mental and physical health
– Not feeling emotionally close to partner during sex
It also found things linked to low interest in sex among women only:
– Having three or more partners in the past year
– Having children under five years old in the household
– Not sharing the same sexual likes and dislikes as partner
Co-author Dr Kirstin Mitchell, at the MRC/CSO Social and Public Health Sciences Unit, University of Glasgow, commented: “The findings on the strong association between open sexual communication and a reduced likelihood of sexual interest problems emphasise the importance of providing a broad sexual and relationships education rather than limiting attention only to adverse consequences of sex and how to prevent them.”
Article: https://medicalxpress.com/news/2017-09-emotional-linked-sexual-problems.html
__________________________________
https://twitter.com/restot50/status/1017506103901421568
https://twitter.com/restot50/status/1005039808824168448
https://twitter.com/Pupucette1/status/1126048125737684992
https://twitter.com/restot50/status/1080515713142587392
https://twitter.com/FleurangeDesir/status/1086494848742510592
https://twitter.com/restot50/status/998666787939078145
https://twitter.com/DannyDPurb/status/955397446959534080
A Prolegomenon to the Construct of the Native Speaker: Heritage Speaker Bilinguals are Natives Too!
Abstract:
This Forum challenges the generally accepted position in the linguistic sciences—conscious or not—that monolingualism and nativeness are essentially synonymous in an exclusive way. We discuss two consequences of our position that naturalistic bilinguals and multilinguals exposed to a language in early childhood are also native speakers: (i) that bi-/multilinguals have multiple native languages; and (ii) nativeness can be applicable to a state of linguistic knowledge that is characterized by significant differences to the monolingual baseline.
Rothman, J. and Treffers-Daller, J. (2014). A Prolegomenon to the Construct of the Native Speaker: Heritage Speaker Bilinguals are Natives Too!. Applied Linguistics, 35(1), pp.93-98.
__________________________________
https://twitter.com/NietzscheAcadem/status/1018514279069298688
__________________________________
Erik Satie – Gnossiennes n°1
Pingback: Essay // Developmental Psychology: The 3 Major Theories of Childhood Development | dpurb . com
Philosophy Review: “The World as Will and Idea”, by Arthur Schopenhauer (1818)
Extract:
Schopenhauer, a pessimistic philosopher, focused on the dark side of life and mental evils and cruelty, which he considered inevitable and that we as psychologists, intellectuals and masters of the mind view as mental disorders that have a negative effect on both the character of the affected and the human environment at large exposed to the vile side of human nature.
This negative view of man’s behaviour and role in life was a sharp contrast to the other more euphoric philosophers who marked the spirits of the generation before him, and who embraced a more idealistic and perhaps a slightly exaggerated euphoric side of man’s mind and character. Though Schopenhauer’s work originally gained little attention at the time it was published [perhaps being too avant-garde for the atavistic institutions of his time], he expressed an interpretation of the world that was dragging and opposed the great ideal of who went before him, such as Victor Schelling and Hegel on some very important points but did not deny expressions of art such as the romantic movement in its various forms.
Schopenhauer who never refrained from publicly criticising people and ideas he disliked was very vocal in his complete contempt for these men, and regarded himself as their great opponent in the ring of the leaders delivering the “Real truth” to mankind and civilisation. Schopenhauer’s work in many ways could be viewed as an extension of another famous German philosopher, namely Immanuel Kant, who preceded him by one generation, delivering his major philosophical work, “a critique of pure reason”. Schopenhauer worked out a system in which reality is known inwardly by a kind of feeling where intellect is only an instrument of the will: the biological will to live and where process rather than result is ultimate.
Schopenhauer’s pessimism lies in his very strong rejection of life. In fact, this rejection is so strong that he even had to address the question of suicide as a solution to life. He fortunately also rejected this “solution” to life, this rejection to life reflected influences with roots in Eastern philosophy, particularly Buddhism, and it is one of the most significant aspects of his work that he was the first Western philosopher to integrate Buddhist thought into Western philosophy. His preoccupation with the evil of the world and the tragedy of life was also somewhat reminiscent of ancient Hindu philosophies. His writings helped to stimulate in Germany an interest in Oriental thought and religion, which can also be seen in the work of many later German philosophers.
In “The World as Will and Idea”, Schopenhauer also considered the important question of the function of art. The value of arts to human life in far more depth than any of his predecessors, and even graded each of the arts, such as music, poetry, architecture [etc], from most important to least important. For that reason, his book had not only a profound effect on future philosophers, but also artists, particularly poets and composers, such as the enigmatic Wagner, who felt indebted to him and sent him a letter of gratitude when he was first introduced to Schopenhauer’s work.
Full Article: https://dpurb.com/2018/08/24/essay-philosophy-review-the-world-as-will-and-idea-by-arthur-schopenhauer-1818/
_____________________
_____________________
_____________________